The impact of the menstrual cycle on emotions and behavior—A review of current research
Abstract
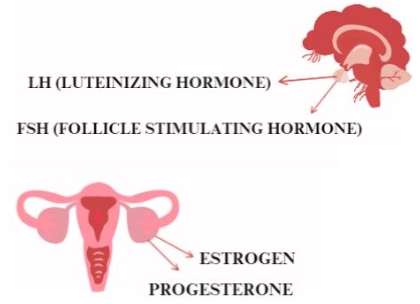
The menstrual cycle has attracted the interest of many researchers for many years. It is analyzed from many angles, including its impact on mental health. Hormonal changes over the course of the cycle have a very strong impact on the emotions, needs, or pain experienced. Estrogen, secreted shortly before ovulation, influences increased confidence and feelings of attractiveness, which can lead to new relationships. In contrast, progesterone, secreted during the luteal phase, promotes the strengthening of stable relationships, and a large proportion of women may experience premenstrual syndrome (PMS) during this time. This publication discusses studies from recent years that have assessed the variability of women’s needs and emerging symptoms during different phases of the cycle. It also summarizes any strategies and practical tips needed to work with women considering their cyclical variability.
References
Ainsworth, A., Peven, K., Bamford, R., et al. (2023). Global Menstrual Cycle Symptomatology as Reported by Users of a Menstrual Tracking Mobile Application. Journal of Psychology p. 20-35 https://doi.org/10.21203/rs.3.rs-3087510/v1
Allen, T. D., Johnson, R. C., Kiburz, K. M., et al. (2012). Work–Family Conflict and Flexible Work Arrangements: Deconstructing Flexibility. Personnel Psychology, 66(2), 345–376. https://doi.org/10.1111/peps.12012
Beníčková, M., Gimunová, M., Paludo, A. C. (2024). Effect of circadian rhythm and menstrual cycle on physical performance in women: a systematic review. Frontiers in Physiology, 15. https://doi.org/10.3389/fphys.2024.1347036
Bernal, A., and Paolieri, D. (2022). The influence of estradiol and progesterone on neurocognition during three phases of the menstrual cycle: Modulating factors. Behavioural Brain Research, 417, 113593. https://doi.org/10.1016/j.bbr.2021.113593
Bhatia, S. C., and Bhatia, S. K. (2002). Diagnosis and treatment of premenstrual dysphoric disorder. American Family Physician, 66(7), 1239–1248.
Bürger, I., Erlandsson, K., and Borneskog, C. (2024). Perceived associations between the menstrual cycle and Attention Deficit Hyperactivity Disorder (ADHD): A qualitative interview study exploring lived experiences. Sexual and Reproductive Healthcare, 40, 100975. https://doi.org/10.1016/j.srhc.2024.100975
Chandra, P. S. (2013). Knowledge about menstruation and reproductive health among adolescent girls in rural India. Journal of Pediatric and Adolescent Gynecology, 26(3), 163-167.
Chrisler, J. C. (2011). Leaks, Lumps, and Lines. Psychology of Women Quarterly, 35(2), 202–214. https://doi.org/10.1177/0361684310397698
Çınar, H. Ü., Kızılkan, M. P., Akalın, A., et al. (2023). Assessing the Menstrual Cycle and Related Problems in Adolescents with a Genetic Syndrome Associated with Intellectual Disability. Journal of Pediatric and Adolescent Gynecology, 36(4), 363–371. https://doi.org/10.1016/j.jpag.2023.02.005
Comasco, E., Frokjaer, V. G., and Sundström-Poromaa, I. (2014). Functional and molecular neuroimaging of menopause and hormone replacement therapy. Frontiers in Neuroscience, 8. https://doi.org/10.3389/fnins.2014.00388
Debruine, L. M. (2005). The impact of hormonal contraceptive use on women’s risk-taking behavior during the ovulatory phase. Evolution and Human Behavior, 26(3), 272-280.
Durante, K. M., Griskevicius, V., Hill, S. E., et al. (2011). Ovulation, Female Competition, and Product Choice: Hormonal Influences on Consumer Behavior. Journal of Consumer Research, 37(6), 921–934. https://doi.org/10.1086/656575
Freeman, E. W. (1995). Efficacy of serotonin reuptake inhibitors in treatment of premenstrual dysphoria: a systematic review and meta-analysis. Archives of Women’s Mental Health, 1(1), 71-79.
Gloe, L. M., Kashy, D. A., Jacobs, E. G., et al. (2021). Examining the role of ovarian hormones in the association between worry and working memory across the menstrual cycle. Psychoneuroendocrinology, 131, 105285. https://doi.org/10.1016/j.psyneuen.2021.105285
Hackney, A. C., Kallman, A. L., and Ağgön, E. (2019). Female sex hormones and the recovery from exercise: Menstrual cycle phase affects responses. Biomedical Human Kinetics, 11(1), 87–89. https://doi.org/10.2478/bhk-2019-0011
Hamidovic, A., Karapetyan, K., Serdarevic, F., et al. (2020). Higher Circulating Cortisol in the Follicular vs. Luteal Phase of the Menstrual Cycle: A Meta-Analysis. Frontiers in Endocrinology, 11. https://doi.org/10.3389/fendo.2020.00311
Handy, A. B., Greenfield, S. F., Yonkers, K. A., et al. (2022). Psychiatric Symptoms Across the Menstrual Cycle in Adult Women: A Comprehensive Review. Harvard Review of Psychiatry, 30(2), 100–117. https://doi.org/10.1097/hrp.0000000000000329
Haselton, M. G., Mortezaie, M., Pillsworth, E. G., et al. (2007). Ovulatory shifts in human female ornamentation: Near ovulation, women dress to impress. Hormones and Behavior, 51(1), 40–45. https://doi.org/10.1016/j.yhbeh.2006.07.007
Hirschberg, A. L. (2012). Sex hormones, appetite and eating behaviour in women. Maturitas, 71(3), 248–256. https://doi.org/10.1016/j.maturitas.2011.12.016
Hoppenbrouwers, K., Roelants, M., Meuleman, C., et al. (2015). Characteristics of the menstrual cycle in 13-year-old Flemish girls and the impact of menstrual symptoms on social life. European Journal of Pediatrics, 175(5), 623–630. https://doi.org/10.1007/s00431-015-2681-7
Hromatko, I., and Mikac, U. (2023). A Mid-Cycle Rise in Positive and Drop in Negative Moods among Healthy Young Women: A Pilot Study. Brain Sciences, 13(1), 105. https://doi.org/10.3390/brainsci13010105
Karali, E., and Gürkan, Ö. C. (2024). Effects of laughter yoga on premenstrual symptoms. Alternative Therapies in Health and Medicine, 30(2), 6-12.
Kvalem, I. L., Dahr Nygaard, I. M., Træen, B., et al. (2024). Menstrual attitudes in adult women: A cross-sectional study on the association with menstruation factors, contraceptive use, genital self-image, and sexual openness. Women’s Health, 20. https://doi.org/10.1177/17455057241249553
Lundin, C., Danielsson, K. G., Bixo, M., et al. (2017). Combined oral contraceptive use is associated with both improvement and worsening of mood in the different phases of the treatment cycle—A double-blind, placebo-controlled randomized trial. Psychoneuroendocrinology, 76, 135–143. https://doi.org/10.1016/j.psyneuen.2016.11.033
Maner, J. K., and Miller, S. L. (2014). Hormones and social monitoring: Menstrual cycle shifts in progesterone underlie women’s sensitivity to social information. Evolution and Human Behavior, 35(1), 9–16. https://doi.org/10.1016/j.evolhumbehav.2013.09.001
Marjoribanks, J., Brown, J., O’Brien, P. M. S., et al. (2013). Selective serotonin reuptake inhibitors for premenstrual syndrome. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.cd001396.pub3
Meers, J. M., Bower, J., Nowakowski, S., et al. (2024). Interaction of sleep and emotion across the menstrual cycle. Journal of Sleep Research. Portico. https://doi.org/10.1111/jsr.14185
Miller, G., Tybur, J. M., and Jordan, B. D. (2007). Ovulatory cycle effects on tip earnings by lap dancers: economic evidence for human estrus?. Evolution and Human Behavior, 28(6), 375–381. https://doi.org/10.1016/j.evolhumbehav.2007.06.002
Monteiro, D. C., Ramos, C. da S., Alves, L. E. N. N., et al. (2024). Functional and structural neuroimaging in premenstrual dysphoric disorder: A systematic review. Journal of Psychiatric Research, 175, 205–210. https://doi.org/10.1016/j.jpsychires.2024.05.024
Nappi, R. E., Cucinella, L., Bosoni, D., et al. (2022). Premenstrual Syndrome and Premenstrual Dysphoric Disorder as Centrally Based Disorders. Endocrines, 3(1), 127–138. https://doi.org/10.3390/endocrines3010012
Neave, N. (2008). Hormones and behavior: The influence of phase of the menstrual cycle on behavioral tendencies. Journal of Neuroendocrinology, 20(5), 683-692.
Passoni, P., Inzoli, A., De Ponti, E., et al. (2024). Association between Physical Activity and Menstrual Cycle Disorders in Young Athletes. International Journal of Sports Medicine, 45(07), 543–548. CLOCKSS. https://doi.org/10.1055/a-2278-3253
Peyrot, C., Provencher, J., Duplessis Marcotte, F., et al. (2024). Using unconditioned responses to predict fear acquisition, fear extinction learning, and extinction retention patterns: Sex hormone status matters. Behavioural Brain Research, 459, 114802. https://doi.org/10.1016/j.bbr.2023.114802
Pletzer, B., and Noachtar, I. (2023). Emotion recognition and mood along the menstrual cycle. Hormones and Behavior, 154, 105406. https://doi.org/10.1016/j.yhbeh.2023.105406
Quaglia, C., Nettore, I. C., Palatucci, G., et al. (2023). Association between Dietary Habits and Severity of Symptoms in Premenstrual Syndrome. International Journal of Environmental Research and Public Health, 20(3), 1717. https://doi.org/10.3390/ijerph20031717
Ramey, E. S. (2023). Tracking Menstrual Cycles for Mood Insight and Suicide Prevention. Journal of Psychosocial Nursing and Mental Health Services, 61(7), 5–6. https://doi.org/10.3928/02793695-20230111-01
Reed, B. G., Carr, B. R., Feingold, K.R.,et al. (editors). (2018). The normal menstrual cycle and the control of ovulation. MDText.com, Inc
Reilly, T. J., Sagnay de la Bastida, V. C., Joyce, D. W., et al. (2019). Exacerbation of Psychosis During the Perimenstrual Phase of the Menstrual Cycle: Systematic Review and Meta-analysis. Schizophrenia Bulletin, 46(1), 78–90. https://doi.org/10.1093/schbul/sbz030
Rogan, M. M., and Black, K. E. (2022). Dietary energy intake across the menstrual cycle: a narrative review. Nutrition Reviews, 81(7), 869–886. https://doi.org/10.1093/nutrit/nuac094
Romans, S., Clarkson, R., Einstein, G., et al. (2012). Mood and the Menstrual Cycle: A Review of Prospective Data Studies. Gender Medicine, 9(5), 361–384. https://doi.org/10.1016/j.genm.2012.07.003
Rugvedh, P., Gundreddy, P., and Wandile, B. (2023). The Menstrual Cycle’s Influence on Sleep Duration and Cardiovascular Health: A Comprehensive Review. Cureus. https://doi.org/10.7759/cureus.47292
Russman Block, S. R., Klump, K. L., Beltz, A. M., et al. (2024). Ovarian hormones reduce the negative association between worry and cognitive control: A combined neural and behavioral investigation. Psychoneuroendocrinology, 161, 106947. https://doi.org/10.1016/j.psyneuen.2023.106947
Schleifenbaum, L., Driebe, J. C., Gerlach, T. M., et al. (2021). Women feel more attractive before ovulation: evidence from a large-scale online diary study. Evolutionary Human Sciences, 3. https://doi.org/10.1017/ehs.2021.44
Souza, M. do C. B. de, Antunes, R. de A., Souza, M. M. de, et al. (2024). Corpus luteum and progesterones in embryo transfer cycles: current challenges of different luteal phase support protocols. JBRA Assisted Reproduction, 28(2). https://doi.org/10.5935/1518-0557.20240044
Sun, Q., Li, G., Zhao, F., et al. (2024). Role of estrogen in treatment of female depression. Aging. https://doi.org/10.18632/aging.205507
Tauseef, H. A., Schmalenberger, K. M., Barone, J. C., et al. (2024). Is trait rumination associated with affective reactivity to the menstrual cycle? A prospective analysis. Psychological Medicine, 54(8), 1824–1834. https://doi.org/10.1017/s0033291723003793
Tiranini, L., and Nappi, R. E. (2022). Recent advances in understanding/management of premenstrual dysphoric disorder/premenstrual syndrome. Faculty Reviews, 11. https://doi.org/10.12703/r/11-11
Uskul, A. K., and Over, H. (2014). Women’s mental health and well-being during the menstrual cycle: The role of perceived social support and self-compassion. Journal of Health Psychology, 19(11), 1343-1351.
Wang, J.X., Zhuang, J.Y., Fu, L., et al. (2021). Social Orientation in the Luteal Phase: Increased Social Feedback Sensitivity, Inhibitory Response, Interpersonal Anxiety and Cooperation Preference. Evolutionary Psychology, 19(1), 147470492098686. https://doi.org/10.1177/1474704920986866
White, T. L. (2017). Hormonal influences on decision making and risk-taking in the menstrual cycle. Journal of Behavioral Decision Making, 30(4), 736-748.
Yi, S. J., Kim, M., and Park, I. (2023). Investigating influencing factors on premenstrual syndrome (PMS) among female college students. BMC Women’s Health, 23(1). https://doi.org/10.1186/s12905-023-02752-y
Yonkers, K. A. (2008). Efficacy of new treatments for premenstrual dysphoric disorder. Journal of Clinical Psychiatry, 69(8), 1144-1152.
Copyright (c) 2024 Magdalena Kurpanik, Maja Grzybowska, Karolina Krupa-Kotara, Katarzyna Barylska, Paweł Juraszek, Mateusz Krystian Grajek

This work is licensed under a Creative Commons Attribution 4.0 International License.