The impact of the presence of hirsutism and hypertrichosis on the psychological state of women suffering from polycystic ovary syndrome and hyperandrogenism
Abstract
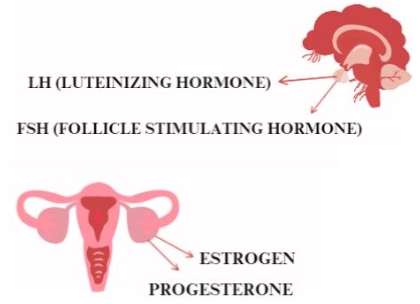
This review article focuses on analyzing the impact of excessive hairiness, in the form of hirsutism and hypertrichosis, on the psychological state of women affected by polycystic ovary syndrome (PCOS) and hyperandrogenism. PCOS is one of the most common endocrine disorders in women, characterized by hyperandrogenism, insulin resistance and menstrual disorders, among others. Studies suggest that excessive body hair can have a significant impact on the quality of life and psychological state of PCOS patients, leading to lowered self-esteem, depression, anxiety and body dysmorphophobia. Despite numerous clinical observations, however, a complete understanding of the mechanisms underlying this association is lacking. The article underscores the need for further research to identify the biological and psychological mechanisms affecting the psychological state of women with excessive body hair in the context of PCOS and hyperandrogenism. As progress is made in this area, it will be possible to develop more effective management strategies and therapeutic interventions that can help improve the quality of life for these patients.
References
Alijanpour, R. (2016). The effect of topical finasteride 0.5% on the outcome of diode laser therapy in the treatment of excess facial hair in the women with hirsutism. J. Pak. Med. Assoc, 66(9), 1107–1110.
Andrzejczak, S. (2020). Hirsutism as a cosmetic problem [PhD thesis]. Jagiellonian University.
Besenek, M., & Gurlek, B. (2020). Hyperandrogenism in polycystic ovary syndrome affects psychological well‐being of adolescents. Journal of Obstetrics and Gynaecology Research, 47(1), 137–146. https://doi.org/10.1111/jog.14444
Błaszczyk, K. (2018). The role of selected adipokines in polycystic ovary syndrome (PCOS) [PhD thesis]. Jagiellonian University.
Bumbuliene, Z., & Alisauskas, J. (2009). Diagnosis and treatment of hirsutism in girls. Gynecology Poland, 80, 374–378.
Ekbäck, M., Wijma, K., & Benzein, E. (2009). “It Is Always on My Mind”: Women’s Experiences of Their Bodies When Living With Hirsutism. Health Care for Women International, 30(5), 358–372. https://doi.org/10.1080/07399330902785133
Elsenbruch, S., Benson, S., Hahn, S., et al. (2006). Determinants of emotional distress in women with polycystic ovary syndrome. Human Reproduction, 21(4), 1092–1099. https://doi.org/10.1093/humrep/dei409
Farkas, J., Rigó, A., & Demetrovics, Z. (2013). Psychological aspects of the polycystic ovary syndrome. Gynecological Endocrinology, 30(2), 95–99. https://doi.org/10.3109/09513590.2013.852530
Franks, S. (2008). Polycystic ovary syndrome in adolescents. International Journal of Obesity, 32(7), 1035–1041. https://doi.org/10.1038/ijo.2008.61
Himelein, M. J., & Thatcher, S. S. (2006). Polycystic Ovary Syndrome and Mental Health: A Review. Obstetrical & Gynecological Survey, 61(11), 723–732. https://doi.org/10.1097/01.ogx.0000243772.33357.84
Imko-Walczuk, B., Cegielska, A., & Glombiowska, M. (2012). Changes in hair distribution in postmenopausal women. Dermatology Review/Dermatology Review, 99(1), 62–67.
Inoue, Y., Nishioka, H., Inukai, M., et al. (2024). What are the Factors That Induce Paradoxical Hypertrichosis After Laser Hair Removal? Aesthetic Surgery Journal, 44(5), NP347–NP353. https://doi.org/10.1093/asj/sjae018
Katulski, K., & Meczekalski, B. (2011). Objective assessment of hyperandrogenism and modern ideas on PCOS treatment. Archives of Perinatal Medicine, 17, 210–216.
Keegan, A., Liao, L.-M., & Boyle, M. (2003). ‘Hirsutism’: A Psychological Analysis. Journal of Health Psychology, 8(3), 327–345. https://doi.org/10.1177/13591053030083004
Kłosowski, P., Świątkowska-Stodulska, R., Berlińska, A., et al. (2017). Hyperandrogenism in postmenopausal women. Forum of Family Medicine, 11(5), 195–208.
Kruk, J. (2021). A dietary strategy for the treatment of polycystic ovary syndrome (PCOS). Journal of NutriLife, 2.
Kurek, G., & Babiarczyk, B. (2017). Bio-psycho-social problems of women of reproductive age with polycystic ovary syndrome. Polish Review of Health Sciences, 50(1), 7–15.
Mallat, F., Chaaya, C., Aoun, M., et al. (2023). Adverse Events of Light-Assisted Hair Removal: An Updated Review. Journal of Cutaneous Medicine and Surgery, 27(4), 375–387. https://doi.org/10.1177/12034754231174852
Marszalec, P. (2021). Analysis of the influence of an anti-inflammatory diet with a low glycemic index on the course and treatment of hyperandrogenism in women of reproductive age [PhD thesis]. Jagiellonian University.
Morgan, J., Scholtz, S., Lacey, H., et al. (2008). The prevalence of eating disorders in women with facial hirsutism: An epidemiological cohort study. International Journal of Eating Disorders, 41(5), 427–431. https://doi.org/10.1002/eat.20527
Mrozińska, S., Kiałka, M., Doroszewska, K., et al. (2015). Hyperandrogenemia of ovarian origin in a postmenopausal woman with associated adrenal adenoma-a case report. Medical Review, 72(7), 387–390.
Nowicki, R., Trzeciak, M., Kaczmarski, M., et al. (2019). Atopic dermatitis. Interdisciplinary diagnostic and therapeutic recommendations of the Polish Dermatological Society, Polish Society of Allergology, Polish Pediatric Society and Polish Society of Family Medicine. Part I. Prophylaxis, topical treatment and phototherapy. Dermatology Review, 106(4), 354–374. https://doi.org/10.5114/dr.2019.88253
Otlewska, A., Hackemer, P., & Menzel, F. (2018). Hirsutism. Pediatria i Medycyna Rodzinna, 14(4), 392–395. https://doi.org/10.15557/pimr.2018.0050
Predota, A., & Imko-Walczuk, B. (2012). Eflornithine-new possibilities in treatment of hirsutism and hypertrichosis. Dermatology Review/Dermatological Review, 99(6), 701–706.
Rodriguez-Paris, D., Remlinger-Molenda, A., Kurzawa, R., et al. (2019). Psychosexual disorders in women with polycystic ovary syndrome. Psychiatr Pol, 53(4), 955–966. https://doi.org/10.12740/PP/OnlineFirst/93105
Rosenfield, R. L. (2005). Hirsutism. New England Journal of Medicine, 353(24), 2578–2588. https://doi.org/10.1056/nejmcp033496
Sadeeqa, S., Mustafa, T., & Latif, S. (2018). Polycystic ovarian syndrome-related depression in adolescent girls: A Review. Journal of pharmacy & bioallied sciences, 10(2), 55–59. https://doi.org/10.4103/JPBS.JPBS_1_18
Saleh, D., Yarrarapu, S. N. S., & Cook, C. (2024). Hypertrichosis. In: StatPearls. StatPearls Publishing.
Scaruffi, E., Franzoi, I. G., Civilotti, C., et al. (2018). Body image, personality profiles and alexithymia in patients with polycystic ovary syndrome (PCOS). Journal of Psychosomatic Obstetrics & Gynecology, 40(4), 294–303. https://doi.org/10.1080/0167482x.2018.1530210
Snast, I., Kaftory, R., Lapidoth, M., et al. (2021). Paradoxical Hypertrichosis Associated with Laser and Light Therapy for Hair Removal: A Systematic Review and Meta-analysis. American Journal of Clinical Dermatology, 22(5), 615–624. https://doi.org/10.1007/s40257-021-00611-w
Sowińska-Przepiera, E., Niedzielska, M., Syrenicz-Maciąg, I., et al. (2018). Hyperandrogenism in women as a clinical, diagnostic and therapeutic problem. Medical Review, 75(8), 405–410.
Stuła, M., Bartholomew, S., & Gawry’s, J. (2019). Effect of oral contraceptives on skin condition. Aesthetic Cosmetology, 8(1), 65–71.
Tłuszcz, K. (2020). Quality of life in women with polycystic ovary syndrome and infertility [PhD thesis]. Jagiellonian University.
Trent, M., Austin, S. B., Rich, M., et al. (2005). Overweight Status of Adolescent Girls With Polycystic Ovary Syndrome: Body Mass Index as Mediator of Quality of Life. Ambulatory Pediatrics, 5(2), 107–111. https://doi.org/10.1367/a04-130r.1
Trzęsowska-Greszta, E., Jastrzębski, J., Sikora, R., et al. (2017). Level of depression in women with impaired procreation vs. stress coping style and psychological gender. Scientific Quarterly Fides et Ratio, 29(1), 191–215.
Vedak, P. (2022). Hair and nail conditions: Hypertrichosis and hirsutism. FP Essent, 517, 22–26.
Wertheim, K., Sobczyńska-Tomaszewska, A., & Bal, J. (2007). Search for the etiopathogenesis of polycystic ovary syndrome (PCOS) (Polish). Ginekologia polska, 78(8), 626–631.
Zdonek, A. (2013). The Clinical manifestations and pharmacotherapy options for policystic ovary syndrome [PhD thesis]. Jagiellonian University.
Ziółkowska, B., & Wróbel, P. (2020). Body image and sense of quality of life in young women with polycystic ovary syndrome. Developmental Psychology, 28(1), 101-113.
Copyright (c) 2024 Martyna Szymanska, Beata Nowak, Karolina Krupa-Kotara, Katarzyna Barylska, Mateusz Grajek

This work is licensed under a Creative Commons Attribution 4.0 International License.