Understanding and role of gut microbiota on drug response and toxicity
Abstract
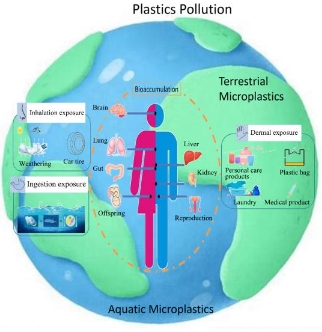
The gut microbiota affects human health profoundly, and evidence is mounting that it can cause, worsen, or resolve illnesses. Particularly in drug-induced toxicity, its role in diverse toxicological reactions has garnered attention recently. Drugs may interact directly or indirectly, through the gut flora, whether or not they are taken orally, changing the toxicity. Current research focuses mainly on the one-way effect of xenobiotics on the makeup and activities of gut microbes, which leads to altered homeostasis. However, there are two-way interactions between the gut microbiota and xenobiotics, and it is important to consider how the gut microbiota affects xenobiotics, particularly medications. Therefore, we emphasise the microbiome, microbial metabolites, and microbial enzymes in this review to emphasise how the gut microbiota affects medication toxicity. To aid in the identification of micro-biologic targets and processes linked to drug toxicity, we establish connections between medications, the microbiome, microbial enzymes or metabolites, drug metabolites, and host toxicological reactions. In addition, a summary and discussion of contemporary mainstream approaches to controlling medication toxicity by microbiota targeting are provided.
References
[1]Leung C, Rivera L, Furness JB, et al. The role of the gut microbiota in NAFLD. Nature Reviews Gastroenterology & Hepatology. 2016; 13(7): 412-425. doi: 10.1038/nrgastro.2016.85
[2]Bäckhed F, Ley RE, Sonnenburg JL, et al. Host‐bacterial mutualism in the human intestine. Science. 2005; 307(80): 1915‐1920. doi: 10.1126/science.1104816
[3]Ley RE, Turnbaugh PJ, Klein S, et al. Microbial ecology: human gut microbes associated with obesity. Nature. 2006; 444: 1022‐1023. doi: 10.1038/4441022a
[4]Seshadri S. Microbial Communication via Quorum Sensing: Influence and Alteration of Gut Ecosystem. JSM Biochemistry and Molecular Biology. 2017; 4(1): 1020-1023.
[5]Mandaliya DK, Seshadri S. Short Chain Fatty Acids, pancreatic dysfunction and type 2 diabetes. Pancreatology. 2019; 19(2): 280-284. doi: 10.1016/j.pan.2019.01.021
[6]Mandaliya DK, Patel S, Seshadri S. The combinatorial effect of acetate and propionate on high fat diet induced diabetic inflammation or metaflammation and T cell polarization. Inflammation 2021; 44: 68-79. doi: 10.1007/s10753-020-01309-7.
[7]Patel S, Seshadri S, Dalai S. Gut microbiome and type 2 diabetes. Progress in Molecular Biology and Translational Science. 2022; 191(1): 175-185. doi: 10.1016/bs.pmbts.2022.06.029
[8]Kumar S, Bhatia Z, Seshadri S. Mapping the Microbial Metabolites in Metabolic Disorder with Special Reference to Type-2 Diabetes. In: Kothari V, Kumar P, Ray S (editors). Probiotics, Prebiotics, Synbiotics, and Postbiotics: Human Microbiome and Human Health. Springer Press; 2023. pp. 67-80. doi: 10.1007/978-981-99-1463-0_4
[9]Nishida A, Inoue R, Inatomi O, et al. Gut microbiota in the pathogenesis of inflammatory bowel disease. Clinical Journal of Gastroenterology. 2018; 11: 1‐10. doi: 10.1007/s12328-017-0813-5
[10]Gorkiewicz G, Moschen A. Gut microbiome: a new player in gastrointestinal disease. Virchows Archiv. 2018; 472: 159‐172. doi: 10.1007/s00428-017-2277-x
[11]Wiest R, Albillos A, Trauner M, et al. Targeting the gut‐liver axis in liver disease. Journal of Hepatology. 2017; 67(5): 1084‐1103. doi: 10.1016/j.jhep.2017.05.007
[12]Bhatia Z, Kumar S, Seshadri S. Exploring the Unexplored Arena: Butyrate as a Dual Communicator in Gut-Brain Axis. In: Kothari V, Kumar P, Ray S (editors). Probiotics, Prebiotics, Synbiotics, and Postbiotics: Human Microbiome and Human Health. Springer Press; 2023. pp. 153-164. doi: 10.1007/978-981-99-1463-0_9
[13]Yang T, Richards EM, Pepine CJ, et al. The gut microbiota and the brain‐gut‐kidney axis in hypertension and chronic kidney disease. Nature Reviews Nephrology. 2018; 14: 442‐456. doi: 10.1038/s41581-018-0018-2
[14]Mancini A, Campagna F, Amodio P, et al. Gut: Liver: brain axis: the microbial challenge in the hepatic encephalopathy. Food & Function. 2018; 9(3): 1373‐1388. doi: 10.1039/c7fo01528c
[15]Stevens JL, Baker TK. The future of drug safety testing: expanding the view and narrowing the focus. Drug Discovery Today. 2009; 14: 162‐167. doi: 10.1016/j.drudis.2008.11.009
[16]Lam KN, Alexander M, Turnbaugh PJ. Precision medicine goes microscopic: engineering the microbiome to improve drug outcomes. Cell Host Microbe. 2019; 26(1): 22‐34. doi: 10.1016/j.chom.2019.06.011
[17]Li H, He J, Jia W. The influence of gut microbiota on drug metabolism and toxicity. Expert Opinion on Drug Metabolism and Toxicology. 2016; 12: 31‐40. doi: 10.1517/17425255.2016.1121234
[18]Collins SL, Patterson AD. The gut microbiome: an orchestrator of xenobiotic metabolism. Acta Pharmaceutica Sinica B 2020; 10: 19‐32. doi: 10.1016/j.apsb.2019.12.001
[19]Zhang J, Zhang J, Wang R. Gut microbiota modulates drug pharmacokinetics. Drug Metabolism Reviews. 2018; 50: 357‐368. doi: 10.1080/03602532.2018.1497647
[20]Li Y, Meng Q, Yang M, et al. Current trends in drug metabolism and pharmacokinetics. Acta Pharmaceutica Sinica B. 2019; 9: 1113‐1144. doi: 10.1016/j.apsb.2019.10.001
[21]Yip LY, Aw CC, Lee SH, et al. The liver-gut microbiota axis modulates hepatotoxicity of tacrine in the rat. Hepatology. 2017; 67(1): 282-295. doi: 10.1002/hep.29327
[22]Relling MV, Evans WE. Pharmacogenomics in the clinic. Nature. 2015; 526(7573): 343-350. doi: 10.1038/nature15817
[23]Zimmermann M, Zimmermann-Kogadeeva M, Wegmann R, et al. Separating host and microbiome contributions to drug pharmacokinetics and toxicity. Science. 2019; 363(6427). doi: 10.1126/science.aat9931
[24]Koppel N, Maini Rekdal V, Balskus EP. Chemical transformation of xenobiotics by the human gut microbiota. Science. 2017; 356(6344). doi: 10.1126/science.aag2770
[25]Wilson ID, Nicholson JK. Gut microbiome interactions with drug metabolism, efficacy, and toxicity. Translational Research. 2017; 179: 204-222. doi: 10.1016/j.trsl.2016.08.002
[26]Clarke G, Sandhu KV, Griffin BT, et al. Gut Reactions: Breaking Down Xenobiotic-Microbiome Interactions. France CP, ed. Pharmacological Reviews. 2019; 71(2): 198-224. doi: 10.1124/pr.118.015768
[27]Carter JH, McLafferty MA, Goldman P. Role of the gastrointestinal microflora in amygdalin (laetrile)‐induced cyanide toxicity. Biochemical Pharmacology. 1980; 29(3): 301‐304. doi: 10.1016/0006-2952(80)90504-3
[28]Zhou YX, Zhang RQ, Rahman K, et al. Diverse Pharmacological Activities and Potential Medicinal Benefits of Geniposide. Evidence-Based Complementary and Alternative Medicine. 2019; 2019: 1-15. doi: 10.1155/2019/4925682
[29]Akao T, Kobashi K, Aburada M. Enzymic Studies on the Animal and Intestinal Bacterial Metabolism of Geniposide. Biological and Pharmaceutical Bulletin. 1994; 17(12): 1573-1576. doi: 10.1248/bpb.17.1573
[30]Kang MJ, Khanal T, Kim HG, et al. Role of metabolism by human intestinal microflora in geniposide-induced toxicity in HepG2 cells. Archives of Pharmacal Research. 2012; 35(4): 733-738. doi: 10.1007/s12272-012-0418-y
[31]Jin MJ, Kim IS, Kim DH, et al. Effects of Intestinal Microbiota on the Bioavailability of Geniposide in Rats. Journal of Agricultural and Food Chemistry. 2014; 62(40): 9632-9636. doi: 10.1021/jf502557f
[32]Rafii F, Cerniglia CE. Reduction of azo dyes and nitroaromatic compounds by bacterial enzymes from the human intestinal tract. Environmental Health Perspectives. 1995; 103(suppl 5): 17-19. doi: 10.1289/ehp.95103s417
[33]Takeno S, Sakai T. Involvement of the intestinal microflora in nitrazepam‐induced teratogenicity in rats and its relationship to nitroreduction. Teratology. 1991; 44(2): 209-214. doi: 10.1002/tera.1420440209
[34]Aiub CAF, Mazzei JL, Pinto LFR, et al. Evaluation of nitroreductase and acetyltransferase participation in N‐nitrosodiethylamine genotoxicity. Chemico-Biological Interactions. 2006; 161: 146-154. doi: 10.1016/j.cbi.2006.03.012
[35]Das KM, Eastwood MA, McManus JPA, et al. The metabolism of salicylazosulphapyridine in ulcerative colitis: I The relationship between metabolites and the response to treatment in inpatients. Gut. 1973; 14(8): 631-636. doi: 10.1136/gut.14.8.631
[36]Chan RP, Pope DJ, Gilbert AP, et al. Studies of two novel sulfasalazine analogs, ipsalazide and balsalazide. Digestive Diseases and Sciences. 1983; 28(7): 609-615. doi: 10.1007/bf01299921
[37]Jarrott B. Tacrine: In vivo veritas. Pharmacological Research. 2017; 116: 29-31. doi: 10.1016/j.phrs.2016.12.033
[38]National Institute of Diabetes and Digestive and Kidney Diseases. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012.
[39]Encarnação JC, Pires AS, Amaral RA, et al. Butyrate, a dietary fiber derivative that improves irinotecan effect in colon cancer cells. The Journal of Nutritional Biochemistry. 2018; 56: 183-192. doi: 10.1016/j.jnutbio.2018.02.018
[40]Yang W, Wei B, Yan R. Amoxapine Demonstrates Incomplete Inhibition of β-Glucuronidase Activity from Human Gut Microbiota. SLAS Discovery. 2018; 23(1): 76-83. doi: 10.1177/2472555217725264
[41]Chamseddine AN, Ducreux M, Armand JP, et al. Intestinal bacterial β‐glucuronidase as a possible predictive biomarker of irinotecan‐induced diarrhea severity. Pharmacology & Therapeutics. 2019; 199: 1-15.
[42]Roberts AB, Wallace BD, Venkatesh MK, et al. Molecular Insights into Microbialβ-Glucuronidase Inhibition to Abrogate CPT-11 Toxicity. Molecular Pharmacology. 2013; 84(2): 208-217. doi: 10.1124/mol.113.085852
[43]Wallace BD, Wang H, Lane KT, et al. Alleviating Cancer Drug Toxicity by Inhibiting a Bacterial Enzyme. Science. 2010; 330(6005): 831-835. doi: 10.1126/science.1191175
[44]Bhatt AP, Pellock SJ, Biernat KA, et al. Targeted inhibition of gut bacterial β-glucuronidase activity enhances anticancer drug efficacy. Proceedings of the National Academy of Sciences. 2020; 117(13): 7374-7381. doi: 10.1073/pnas.1918095117
[45]Wallace BD, Roberts AB, Pollet RM, et al. Structure and Inhibition of Microbiome β-Glucuronidases Essential to the Alleviation of Cancer Drug Toxicity. Chemistry & Biology. 2015; 22(9): 1238-1249. doi: 10.1016/j.chembiol.2015.08.005
[46]Lamba V, Sangkuhl K, Sanghavi K, et al. PharmGKB summary. Pharmacogenetics and Genomics. 2014; 24(1): 73-79. doi: 10.1097/fpc.0000000000000010
[47]Taylor MR, Flannigan KL, Rahim H, et al. Vancomycin relieves mycophenolate mofetil-induced gastrointestinal toxicity by eliminating gut bacterial β-glucuronidase activity. Science Advances. 2019; 5(8). doi: 10.1126/sciadv.aax2358
[48]Weng ZM, Wang P, Ge GB, et al. Structure-activity relationships of flavonoids as natural inhibitors against E. coli β-glucuronidase. Food and Chemical Toxicology. 2017; 109: 975-983. doi: 10.1016/j.fct.2017.03.042
[49]Awolade P, Cele N, Kerru N, et al. Therapeutic significance of β-glucuronidase activity and its inhibitors: A review. European Journal of Medicinal Chemistry. 2020; 187: 111921. doi: 10.1016/j.ejmech.2019.111921
[50]van Kessel SP, Frye AK, El-Gendy AO, et al. Gut bacterial tyrosine decarboxylases restrict levels of levodopa in the treatment of Parkinson’s disease. Nature Communications. 2019; 10(1). doi: 10.1038/s41467-019-08294-y
[51]Maini Rekdal V, Bess EN, Bisanz JE, et al. Discovery and inhibition of an interspecies gut bacterial pathway for Levodopa metabolism. Science. 2019; 364(6445). doi: 10.1126/science.aau6323
[52]Dobkin JF, Saha JR, Butler VP, et al. Digoxin-Inactivating Bacteria: Identification in Human Gut Flora. Science. 1983; 220(4594): 325-327. doi: 10.1126/science.6836275
[53]Haiser HJ, Gootenberg DB, Chatman K, et al. Predicting and Manipulating Cardiac Drug Inactivation by the Human Gut Bacterium Eggerthella lenta. Science. 2013; 341(6143): 295-298. doi: 10.1126/science.1235872
[54]Yan A, Culp E, Perry J, et al. Transformation of the Anticancer Drug Doxorubicin in the Human Gut Microbiome. ACS Infectious Diseases. 2017; 4(1): 68-76. doi: 10.1021/acsinfecdis.7b00166
[55]Isokpehi RD, Udensi UK, Simmons SS, et al. Evaluative Profiling of Arsenic Sensing and Regulatory Systems in the Human Microbiome Project Genomes. Microbiology Insights. 2014; 7: 25-34. doi: 10.4137/mbi.s18076
[56]Chi L, Xue J, Tu P, et al. Gut microbiome disruption altered the biotransformation and liver toxicity of arsenic in mice. Archives of Toxicology. 2018; 93(1): 25-35. doi: 10.1007/s00204-018-2332-7
[57]Coryell M, McAlpine M, Pinkham NV, et al. The gut microbiome is required for full protection against acute arsenic toxicity in mouse models. Nature Communications 2018; 9: 5424.
[58]Toda T, Saito N, Ikarashi N, et al. Intestinal flora induces the expression of Cyp3a in the mouse liver. Xenobiotica. 2009; 39(4): 323-334. doi: 10.1080/00498250802651984
[59]Björkholm B, Bok CM, Lundin A, et al. Intestinal Microbiota Regulate Xenobiotic Metabolism in the Liver. PLoS ONE. 2009; 4(9): e6958. doi: 10.1371/journal.pone.0006958
[60]Selwyn FP, Cheng SL, Bammler TK, et al. Developmental Regulation of Drug-Processing Genes in Livers of Germ-Free Mice. Toxicological Sciences. 2015; 147(1): 84-103. doi: 10.1093/toxsci/kfv110
[61]Illés P, Krasulová K, Vyhlídalová B, et al. Indole microbial intestinal metabolites expand the repertoire of ligands and agonists of the human pregnane X receptor. Toxicological Letters. 2020; 334: 87‐93. doi: 10.1016/j.toxlet.2020.09.015
[62]Dvořák Z, Sokol H, Mani S. Drug Mimicry: Promiscuous Receptors PXR and AhR, and Microbial Metabolite Interactions in the Intestine. Trends in Pharmacological Sciences. 2020; 41(12): 900-908. doi: 10.1016/j.tips.2020.09.013
[63]Zhang J, Zhu S, Ma N, et al. Metabolites of microbiota response to tryptophan and intestinal mucosal immunity: A therapeutic target to control intestinal inflammation. Medicinal Research Reviews. 2020; 41(2): 1061-1088. doi: 10.1002/med.21752
[64]Dvořák Z, Kopp F, Costello CM, et al. Targeting the pregnane X receptor using microbial metabolite mimicry. EMBO Molecular Medicine. 2020; 12(4). doi: 10.15252/emmm.201911621
[65]Wang D, Li D, Zhang Y, et al. Functional metabolomics reveal the role of AHR/GPR35 mediated kynurenic acid gradient sensing in chemotherapy-induced intestinal damage. Acta Pharmaceutica Sinica B. 2021; 11(3): 763-780. doi: 10.1016/j.apsb.2020.07.017
[66]Xiao H wen, Cui M, Li Y, et al. Gut microbiota-derived indole 3-propionic acid protects against radiation toxicity via retaining acyl-CoA-binding protein. Microbiome. 2020; 8(1). doi: 10.1186/s40168-020-00845-6
[67]Caparrós-Martín JA, Lareu RR, Ramsay JP, et al. Statin therapy causes gut dysbiosis in mice through a PXR-dependent mechanism. Microbiome. 2017; 5(1). doi: 10.1186/s40168-017-0312-4
[68]Seshadri S, Rapaka N, Prajapati B, et al. Statins exacerbate glucose intolerance and hyperglycemia in a high sucrose fed rodent model. Scientific Reports. 2019; 9(1). doi: 10.1038/s41598-019-45369-8
[69]Gwag T, Meng Z, Sui Y, et al. Non‐nucleoside reverse transcriptase inhibitor efavirenz activates PXR to induce hypercholesterolemia and hepatic steatosis. Journal of Hepatology. 2019; 70: 930‐940. doi: 10.1016/j.jhep.2018.12.038
[70]Kansanen E, Kuosmanen SM, Leinonen H, et al. The Keap1-Nrf2 pathway: Mechanisms of activation and dysregulation in cancer. Redox Biology. 2013; 1(1): 45-49. doi: 10.1016/j.redox.2012.10.001
[71]Saeedi BJ, Liu KH, Owens JA, et al. Gut-Resident Lactobacilli Activate Hepatic Nrf2 and Protect Against Oxidative Liver Injury. Cell Metabolism. 2020; 31(5): 956-968. doi: 10.1016/j.cmet.2020.03.006
[72]Thaiss CA, Levy M, Korem T, et al. Microbiota diurnal rhythmicity programs host transcriptome oscillations. Cell. 2016; 167(6): 1495‐1510. doi: 10.1016/j.cell.2016.11.003
[73]Bridgeman SC, Northrop W, Melton PE, et al. Butyrate generated by gut microbiota and its therapeutic role in metabolic syndrome. Pharmacological Research. 2020; 160: 105174. doi: 10.1016/j.phrs.2020.105174
[74]Jia W, Xie G, Jia W. Bile acid-microbiota crosstalk in gastrointestinal inflammation and carcinogenesis. Nature Reviews Gastroenterology & Hepatology. 2017; 15(2): 111-128. doi: 10.1038/nrgastro.2017.119
[75]Garcia-Cortes M, Robles-Diaz M, Stephens C, et al. Drug induced liver injury: an update. Archives of Toxicology. 2020; 94(10): 3381-3407. doi: 10.1007/s00204-020-02885-1
[76]Mowat AMcI. To respond or not to respond — a personal perspective of intestinal tolerance. Nature Reviews Immunology. 2018; 18(6): 405-415. doi: 10.1038/s41577-018-0002-x
[77]Sun D, Bai R, Zhou W, et al. Angiogenin maintains gut microbe homeostasis by balancing α-Proteobacteria and Lachnospiraceae. Gut. 2020; 70(4): 666-676. doi: 10.1136/gutjnl-2019-320135
[78]Chu H, Mazmanian SK. Innate immune recognition of the microbiota promotes host-microbial symbiosis. Nature Immunology. 2013; 14(7): 668-675. doi: 10.1038/ni.2635
[79]Prajapati B, Jena P, Rajput P, et al. Understanding and Modulating the Toll Like Receptors (TLRs) and NOD Like Receptors (NLRs) Cross Talk in Type 2 Diabetes. Current Diabetes Reviews. 2014; 10(3): 190-200. doi: 10.2174/1573399810666140515112609
[80]Deguine J, Barton GM. MyD88: a central player in innate immune signaling. F1000Prime Reports. 2014; 6. doi: 10.12703/p6-97
[81]Kawai T, Adachi O, Ogawa T, et al. Unresponsiveness of MyD88‐deficient mice to endotoxin. Immunity 1999; 11: 115‐122. doi: 10.1016/S1074-7613(00)80086-2
[82]Broz P, Dixit VM. Inflammasomes: mechanism of assembly, regulation and signalling. Nature Reviews Immunology. 2016; 16(7): 407-420. doi: 10.1038/nri.2016.58
[83]Elinav E, Strowig T, Kau AL, et al. NLRP6 Inflammasome Regulates Colonic Microbial Ecology and Risk for Colitis. Cell. 2011; 145(5): 745-757. doi: 10.1016/j.cell.2011.04.022
[84]Seo SU, Kamada N, Muñoz-Planillo R, et al. Distinct Commensals Induce Interleukin-1β via NLRP3 Inflammasome in Inflammatory Monocytes to Promote Intestinal Inflammation in Response to Injury. Immunity. 2015; 42(4): 744-755. doi: 10.1016/j.immuni.2015.03.004
[85]Krishnan S, Ding Y, Saedi N, et al. Gut Microbiota-Derived Tryptophan Metabolites Modulate Inflammatory Response in Hepatocytes and Macrophages. Cell Reports. 2018; 23(4): 1099-1111. doi: 10.1016/j.celrep.2018.03.109
[86]Wei Y, Zeng B, Chen J, et al. Enterogenous bacterial glycolipids are required for the generation of natural killer T cells mediated liver injury. Scientific Reports. 2016; 6(1). doi: 10.1038/srep36365
[87]Peterson DA, McNulty NP, Guruge JL, et al. IgA Response to Symbiotic Bacteria as a Mediator of Gut Homeostasis. Cell Host & Microbe. 2007; 2(5): 328-339. doi: 10.1016/j.chom.2007.09.013
[88]Furusawa Y, Obata Y, Fukuda S, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013; 504(7480): 446-450. doi: 10.1038/nature12721
[89]Arpaia N, Campbell C, Fan X, et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature. 2013; 504(7480): 451-455. doi: 10.1038/nature12726
[90]Singh N, Gurav A, Sivaprakasam S, et al. Activation of Gpr109a, Receptor for Niacin and the Commensal Metabolite Butyrate, Suppresses Colonic Inflammation and Carcinogenesis. Immunity. 2014; 40(1): 128-139. doi: 10.1016/j.immuni.2013.12.007
[91]Schluter J, Peled JU, Taylor BP, et al. The gut microbiota is associated with immune cell dynamics in humans. Nature. 2020; 588(7837): 303-307. doi: 10.1038/s41586-020-2971-8
Copyright (c) 2024 Sriram Seshadri, Devanshi Gajjar, Aneri Joshi, Zeel Bhatia, Sunny Kumar

This work is licensed under a Creative Commons Attribution 4.0 International License.