Threats of nano/microplastics to reproduction and offspring: Potential mechanisms and perspectives
Abstract
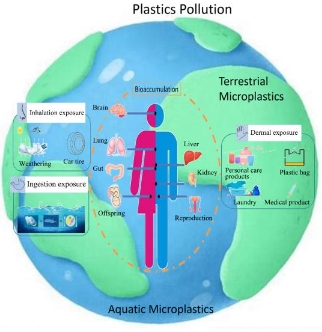
Due to their ubiquitous occurrence in the aquatic environment and terrestrial ecosystem and underlying eco-environmental risks, nano/microplastics (NPs/MPs) have sparked great public concerns. The purpose of this work is aimed to summarize the harmful influence of NPs/MPs on reproduction and offspring health and further explore the potential mechanisms of action, thereby facilitating the more comprehensive understanding of NPs/MPs features. Literature search databases included EMBASE, Web of Science, and PubMed. The study selection and data extraction were implemented according to the inclusion criteria. NPs/MPs could accumulate and trigger reproductive toxic responses and thereafter generate deleterious effects on the offspring's health. Accordingly, the reproductive toxicity of NPs/MPs was characterized as the sperm deformity, decline in sperm count and motility, follicular growth tardiness, ovarian fibrosis, granulosa cell death, disorder of reproductive hormone secretion, as well as the fetal growth restriction, glycolipid metabolism disorder, and inflammatory responses of the next generation. Additionally, mechanism research revealed that NPs/MPs exposure brought about inflammatory responses and oxidative stress and thereafter destroyed the blood-testis barrier (BTB) integrity, motivated spermatogenic cell apoptosis by activating the JNK and p38/MAPK-Nrf2/NF-κB pathways, and induced ovarian granulosa cell pyroptosis and apoptosis and subsequent ovarian fibrosis via the Wnt/β-Catenin and NLRP3/Caspase-1 pathways. Nevertheless, this work also highlighted the imperative requirements for scientific and systematic risk assessments of NPs/MPs, so as to identify feasible risk mitigation strategies.
References
[1]D’Angelo S, Meccariello R. Microplastics: A Threat for Male Fertility. International Journal of Environmental Research and Public Health. 2021; 18(5): 2392. doi: 10.3390/ijerph18052392
[2]Feng Y, Tu C, Li R, et al. A systematic review of the impacts of exposure to micro- and nano-plastics on human tissue accumulation and health. Eco-Environment & Health. 2023; 2(4): 195-207. doi: 10.1016/j.eehl.2023.08.002
[3]Allen S, Allen D, Phoenix VR, et al. Atmospheric transport and deposition of microplastics in a remote mountain catchment. Nature Geoscience. 2019; 12(5): 339-344. doi: 10.1038/s41561-019-0335-5
[4]Wen S, Chen Y, Tang Y, et al. Male reproductive toxicity of polystyrene microplastics: Study on the endoplasmic reticulum stress signaling pathway. Food and Chemical Toxicology. 2023; 172: 113577. doi: 10.1016/j.fct.2022.113577
[5]Abbasi S, Turner A. Human exposure to microplastics: A study in Iran. Journal of Hazardous Materials. 2021; 403: 123799. doi: 10.1016/j.jhazmat.2020.123799
[6]Ibrahim YS, Tuan Anuar S, Azmi AA, et al. Detection of microplastics in human colectomy specimens. JGH Open. 2020; 5(1): 116-121. doi: 10.1002/jgh3.12457
[7]Schwabl P, Köppel S, Königshofer P, et al. Detection of Various Microplastics in Human Stool. Annals of Internal Medicine. 2019; 171(7): 453-457. doi: 10.7326/m19-0618
[8]Yang J, Kamstra J, Legler J, et al. The impact of microplastics on female reproduction and early life. Animal Reproduction. 2023; 20(2). doi: 10.1590/1984-3143-ar2023-0037
[9]Zhao Q, Zhu L, Weng J, et al. Detection and characterization of microplastics in the human testis and semen. Science of The Total Environment. 2023; 877: 162713. doi: 10.1016/j.scitotenv.2023.162713
[10]Senathirajah K, Attwood S, Bhagwat G, et al. Estimation of the mass of microplastics ingested—A pivotal first step towards human health risk assessment. Journal of Hazardous Materials. 2021; 404: 124004. doi: 10.1016/j.jhazmat.2020.124004
[11]Mohamed Nor NH, Kooi M, Diepens NJ, et al. Lifetime Accumulation of Microplastic in Children and Adults. Environmental Science & Technology. 2021; 55(8): 5084-5096. doi: 10.1021/acs.est.0c07384
[12]Pasquini E, Ferrante F, Passaponti L, et al. Microplastics reach the brain and interfere with honey bee cognition. Science of The Total Environment. 2024; 912: 169362. doi: 10.1016/j.scitotenv.2023.169362
[13]Cao J, Xu R, Geng Y, et al. Exposure to polystyrene microplastics triggers lung injury via targeting toll-like receptor 2 and activation of the NF-κB signal in mice. Environmental Pollution. 2023; 320: 121068. doi: 10.1016/j.envpol.2023.121068
[14]Li A, Wang Y, Kulyar MF e A, et al. Environmental microplastics exposure decreases antioxidant ability, perturbs gut microbial homeostasis and metabolism in chicken. Science of The Total Environment. 2023; 856: 159089. doi: 10.1016/j.scitotenv.2022.159089
[15]Wang S, Wu H, Shi X, et al. Polystyrene microplastics with different sizes induce the apoptosis and necroptosis in liver through the PTEN/PI3K/AKT/autophagy axis. Science of The Total Environment. 2023; 899: 165461. doi: 10.1016/j.scitotenv.2023.165461
[16]Xiong X, Gao L, Chen C, et al. The microplastics exposure induce the kidney injury in mice revealed by RNA-seq. Ecotoxicology and Environmental Safety. 2023; 256: 114821. doi: 10.1016/j.ecoenv.2023.114821
[17]Yang S, Li M, Kong RYC, et al. Reproductive toxicity of micro- and nanoplastics. Environment International. 2023; 177: 108002. doi: 10.1016/j.envint.2023.108002
[18]Pereira R, Sousa M. Morphological and Molecular Bases of Male Infertility: A Closer Look at Sperm Flagellum. Genes. 2023; 14(2): 383. doi: 10.3390/genes14020383
[19]Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Available online: https://www.bmj.com/content/bmj/372/bmj.n71.full.pdf (accessed on 14 February 2024).
[20]Hooijmans CR, Rovers MM, de Vries RB, et al. SYRCLE’s risk of bias tool for animal studies. BMC Medical Research Methodology. 2014; 14(1). doi: 10.1186/1471-2288-14-43
[21]Amereh F, Babaei M, Eslami A, et al. The emerging risk of exposure to nano(micro)plastics on endocrine disturbance and reproductive toxicity: From a hypothetical scenario to a global public health challenge. Environmental Pollution. 2020; 261: 114158. doi: 10.1016/j.envpol.2020.114158
[22]Xie X, Deng T, Duan J, et al. Exposure to polystyrene microplastics causes reproductive toxicity through oxidative stress and activation of the p38 MAPK signaling pathway. Ecotoxicology and Environmental Safety. 2020; 190: 110133. doi: 10.1016/j.ecoenv.2019.110133
[23]Ijaz MU, Shahzadi S, Samad A, et al. Dose-Dependent Effect of Polystyrene Microplastics on the Testicular Tissues of the Male Sprague Dawley Rats. Dose-Response. 2021; 19(2): 155932582110198. doi: 10.1177/15593258211019882
[24]Li S, Wang Q, Yu H, et al. Polystyrene microplastics induce blood–testis barrier disruption regulated by the MAPK-Nrf2 signaling pathway in rats. Environmental Science and Pollution Research. 2021; 28(35): 47921-47931. doi: 10.1007/s11356-021-13911-9
[25]Hou B, Wang F, Liu T, et al. Reproductive toxicity of polystyrene microplastics: In vivo experimental study on testicular toxicity in mice. Journal of Hazardous Materials. 2021; 405: 124028. doi: 10.1016/j.jhazmat.2020.124028
[26]Wei Z, Wang Y, Wang S, et al. Comparing the effects of polystyrene microplastics exposure on reproduction and fertility in male and female mice. Toxicology. 2022; 465: 153059. doi: 10.1016/j.tox.2021.153059
[27]Jin H, Yan M, Pan C, et al. Chronic exposure to polystyrene microplastics induced male reproductive toxicity and decreased testosterone levels via the LH-mediated LHR/cAMP/PKA/StAR pathway. Particle and Fibre Toxicology. 2022; 19(1). doi: 10.1186/s12989-022-00453-2
[28]Wen S, Zhao Y, Liu S, et al. Microplastics-perturbed gut microbiota triggered the testicular disorder in male mice: Via fecal microbiota transplantation. Environmental Pollution. 2022; 309: 119789. doi: 10.1016/j.envpol.2022.119789
[29]Jin H, Ma T, Sha X, et al. Polystyrene microplastics induced male reproductive toxicity in mice. Journal of Hazardous Materials. 2021; 401: 123430. doi: 10.1016/j.jhazmat.2020.123430
[30]An R, Wang X, Yang L, et al. Polystyrene microplastics cause granulosa cells apoptosis and fibrosis in ovary through oxidative stress in rats. Toxicology. 2021; 449: 152665. doi: 10.1016/j.tox.2020.152665
[31]Hou J, Lei Z, Cui L, et al. Polystyrene microplastics lead to pyroptosis and apoptosis of ovarian granulosa cells via NLRP3/Caspase-1 signaling pathway in rats. Ecotoxicology and Environmental Safety. 2021; 212: 112012. doi: 10.1016/j.ecoenv.2021.112012
[32]Liu Z, Zhuan Q, Zhang L, et al. Polystyrene microplastics induced female reproductive toxicity in mice. Journal of Hazardous Materials. 2022; 424: 127629. doi: 10.1016/j.jhazmat.2021.127629
[33]Aghaei Z, Sled JG, Kingdom JC, et al. Maternal exposure to polystyrene micro- and nanoplastics causes fetal growth restriction in mice. Environmental Science & Technology Letters. 2022; 9: 426-430. doi: 10.1021/acs.estlett.2c00186
[34]Chen G, Xiong S, Jing Q, et al. Maternal exposure to polystyrene nanoparticles retarded fetal growth and triggered metabolic disorders of placenta and fetus in mice. Science of The Total Environment. 2023; 854: 158666. doi: 10.1016/j.scitotenv.2022.158666
[35]Huang T, Zhang W, Lin T, et al. Maternal exposure to polystyrene nanoplastics during gestation and lactation induces hepatic and testicular toxicity in male mouse offspring. Food and Chemical Toxicology. 2022; 160: 112803. doi: 10.1016/j.fct.2021.112803
[36]Interdonato L, Siracusa R, Fusco R, et al. Endocrine Disruptor Compounds in Environment: Focus on Women’s Reproductive Health and Endometriosis. International Journal of Molecular Sciences. 2023; 24(6): 5682. doi: 10.3390/ijms24065682
[37]Ragusa A, Svelato A, Santacroce C, et al. Plasticenta: First evidence of microplastics in human placenta. Environment International. 2021; 146: 106274. doi: 10.1016/j.envint.2020.106274
[38]Amereh F, Amjadi N, Mohseni-Bandpei A, et al. Placental plastics in young women from general population correlate with reduced foetal growth in IUGR pregnancies. Environmental Pollution. 2022; 314: 120174. doi: 10.1016/j.envpol.2022.120174
[39]Krakowiak P, Smith EN, de Bruyn G, et al. Risk Factors and Outcomes Associated with a Short Umbilical Cord. Obstetrics & Gynecology. 2004; 103(1): 119-127. doi: 10.1097/01.aog.0000102706.84063.c7
[40]Marcelino RC, Cardoso RM, Domingues ELBC, et al. The emerging risk of microplastics and nanoplastics on the microstructure and function of reproductive organs in mammals: A systematic review of preclinical evidence. Life Sciences. 2022; 295: 120404. doi: 10.1016/j.lfs.2022.120404
Copyright (c) 2024 Mei Ha, Wanzhen Tang, Jichun Huang, Changjiang Liu

This work is licensed under a Creative Commons Attribution 4.0 International License.