Nanomaterials in drug delivery—Promises and limitations
Abstract
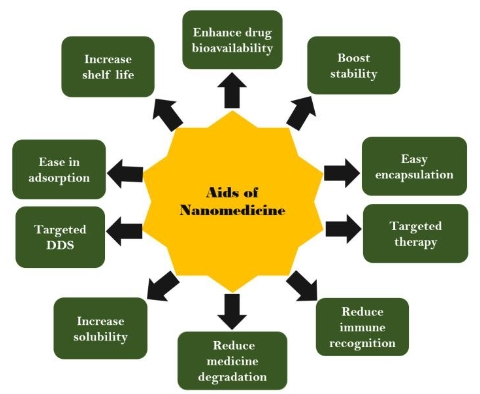
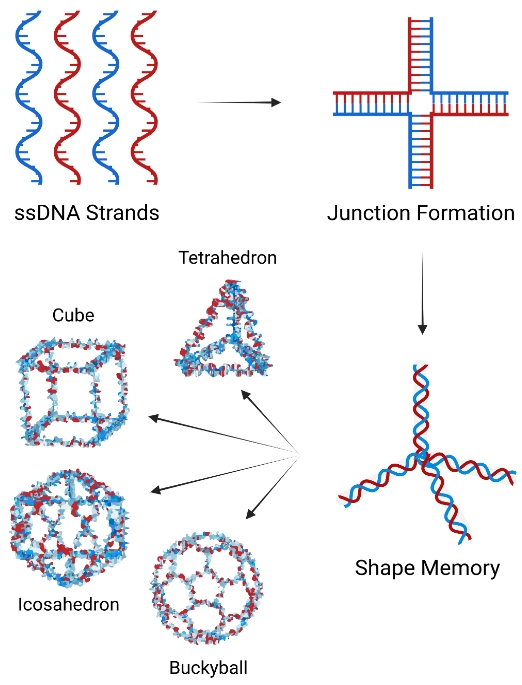
The unprecedented upsurge of human suffering, whose canvas seems to broaden by the emergence of incurable diseases as a result of evolution of novel strains of microbes is further compounded by the development of antimicrobial resistance, growing urbanization and lifestyle. Nanomaterials are of nano size-ranging from 10–100 nm, and nowadays, they are finding immense applications in drug delivery owing to their advantages over the conventional drug delivery systems. This review article aims to discuss various types of nanomaterials including polymeric nanoparticles (polymersomes, dendrimers, polymer micelles, nanospheres, and nanogels), inorganic nanoparticles (SiNPs, quantum dots, MXenes, FeONPs, and AuNPs) and lipid-based nanomaterials (liposome, lipid nanoparticles, emulsions, and niosomes) in drug delivery applications. Besides this, the manuscript also discusses their limitations, suitability, theranostics, and safety concerns in drug delivery. From the discussion about their applications and limitations in drug delivery, it can be conclusively stated that because of their versatility, the nanomaterials are promising contenders in the field of nanomedicine and their utility in healthcare has convincingly endorsed the fact that however ‘nano’ the dimensions of nanomaterials are, they have colossal relevance.
References
[1]Gao W, Zhang L. Nanomaterials arising amid antibiotic resistance. Nature Reviews Microbiology 2021; 19(1): 5–6. doi: 10.1038/s41579-020-00469-5.
[2]Selvarajan V, Obuobi S, Ee PLR. Silica nanoparticles—A versatile tool for the treatment of bacterial infections. Frontiers in Chemistry 2020; 8: 602. doi: 10.3389/fchem.2020.00602.
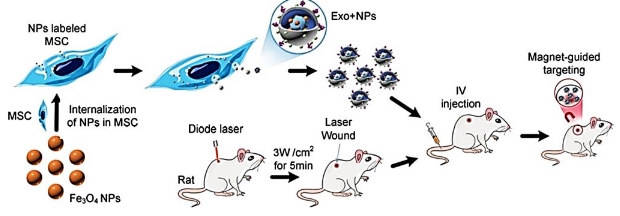
[3]Hooshmand S, Hayat SMG, Ghorbani A, et al. Preparation and applications of superparamagnetic iron oxide nanoparticles in novel drug delivery systems: An overview article. Current Medicinal Chemistry 2021; 28(4): 777–799. doi: 10.2174/0929867327666200123152006.
[4]Karimi M, Mansouri MR, Rabiee N, et al. Advances in nanomaterials for drug delivery. Morgan and Claypool Publishers 2023; 11(2): 399. doi: 10.3390/biomedicines11020399.
[5]Baskin J, Jeon JE, Lewis SJ. Nanoparticles for drug delivery in Parkinson’s disease. Journal of Neurology 2020; 268(5): 1981–1994. doi: 10.1007/s00415-020-10291-x.
[6]Stubelius A, Lee S, Almutairi A. The chemistry of boronic acids in nanomaterials for drug delivery. Accounts of Chemical Research 2019; 52(11): 3108–3119. doi: 10.1021/acs.accounts.9b00292.
[7]De Jong WH, Borm PJ. Drug delivery and nanoparticles: Applications and hazards. International Journal of Nanomedicine 2008; 3(2): 133–149. doi: 10.2147/ijn.s596.
[8]Mandal AK. Dendrimers in targeted drug delivery applications: A review of diseases and cancer. International Journal of Polymeric Materials and Polymeric Biomaterials 2021; 70(4): 287–297. doi: 10.1080/00914037.2020.1713780.
[9]Mirza Z, Karim S. Nanoparticles-based drug delivery and gene therapy for breast cancer: Recent advancements and future challenges. Seminars in Cancer Biology 2021; 69: 226–237. doi: 10.1016/j.semcancer.2019.10.020.
[10]Nagaraju GP, Srivani G, Dariya B, et al. Nanoparticles guided drug delivery and imaging in gastric cancer. Seminars in Cancer Biology 2021; 69: 69–76. doi: 10.1016/j.semcancer.2020.01.006.
[11]Jaudoin C, Agnely F, Nguyen Y, et al. Nanocarriers for drug delivery to the inner ear: Physicochemical key parameters, biodistribution, safety and efficacy. International Journal of Pharmaceutics 2021; 592: 120038. doi: 10.1016/j.ijpharm.2020.120038.
[12]Battaglia L, Gallarate M. Lipid nanoparticles: State of the art, new preparation methods and challenges in drug delivery. Expert Opinion on Drug Delivery 2012; 9(5): 497–508. doi: 10.1517/17425247.2012.673278.
[13]Gyanani V, Haley JC, Goswami R. Challenges of current anticancer treatment approaches with focus on liposomal drug delivery systems. Pharmaceuticals 2021; 14(9): 835. doi: 10.3390/ph14090835.
[14]Jager E, Sincari V, Albuquerque LJ, et al. Reactive oxygen species (ROS)-responsive polymersomes with site-specific chemotherapeutic delivery into tumors via spacer design chemistry. Biomacromolecules 2020; 21(4): 1437–1449. doi: 10.1021/acs.biomac.9b01748.
[15]Yadav HK, Almokdad AA, Sumia IM, et al. Polymer-based nanomaterials for drug-delivery carriers. 1st ed. In: Mohapatra S, Ranjan S, Dasgupta N, et al. (editors). Nanocarriers for drug delivery, nanoscience and nanotechnology in drug delivery, micro and nano technologies. Amsterdam: Elsevier; 2018. p. 531–556.
[16]Güven E. Nanotechnology-based drug delivery systems in orthopedics. Joint Diseases and Related Surgery 2021; 32(1): 267–273. doi: 10.5606/ehc.2021.80360.
[17]Jermy BR, Ravinayagam V, Almohazey D, et al. PEGylated green halloysite/spinel ferrite nanocomposites for pH sensitive delivery of dexamethasone: A potential pulmonary drug delivery treatment option for COVID-19. Applied Clay Science 2022; 216: 106333. doi: 10.1016/j.clay.2021.106333.
[18]Lomis N, Sarfaraz ZK, Alruwaih A, et al. Albumin nanoparticle formulation for heart-targeted drug delivery: In vivo assessment of congestive heart failure. Pharmaceuticals 2021; 14(7): 697. doi: 10.3390/ph14070697.
[19]Liu Y, Zhu S, Gu Z, et al. Toxicity of manufactured nanomaterials. Particuology 2022; 69: 31–48. doi: 10.1016/j.partic.2021.11.007.
[20]Kyriakides TR, Raj A, Tseng TH, et al. Biocompatibility of nanomaterials and their immunological properties. Biomedical Materials 2021; 16(4): 042005. doi: 10.1088/1748-605X/abe5fa.
[21]Singh R, Sharma A, Saji J, et al. Smart nanomaterials for cancer diagnosis and treatment. Nano Convergence 2022; 9(1): 21. doi: 10.1186/s40580-022-00313-x.
[22]Ranjha MMAN, Shafique B, Rehman A, et al. Biocompatible nanomaterials in food science, technology, and nutrient drug delivery: Recent developments and applications. Frontiers in Nutrition 2022; 8: 1141. doi: 10.3389/fnut.2021.778155.
[23]Jha AK, Kumari N, Kumari P, et al. Phytochemical synthesis of ZnO nanoparticles: Antimicrobial and anticancer activity. Journal of Bionanosciences 2018; 12(6): 836–841. doi: 10.1166/jbns.2018.1601.
[24]Jha AK, Prasad K. Green synthesis of silver nanoparticles and its activity on SiHa cervical cancer cell line. Advanced Materials Letters 2014; 5(9): 501–505. doi: 10.5185/amlett.2014.4563.
[25]Jha AK, Prasad K. Platinum nanoparticles: Biosynthesis and activity on SiHa cervical cancer cell line. Indian Journal of Biotechnology 2017; 16: 536–541.
[26]Kumari P, Kumari N, Singh KP, et al. Cymbopogon flexuosus leaves mediated synthesis of ZnO nanoparticles: Cytotoxicity assay against THP-1 human leukemia cell line. Journal of Bionanoscience 2018; 12(5): 683–688. doi: 10.1166/jbns.2018.1571.
[27]Jha B, Zamani S, Jha AK, et al. Biogenic platinum as nanomedicine: A synergism of ethnomedicine and nanotechnology. Bioscience Biotechnology Research Communications 2020; 13(4): 2157–2162. doi: 10.21786/bbrc/13.4/79.
[28]Kumari N, Kumari P, Jha AK, Prasad K. Medicinal plants derived silver nanoparticles: Cytotoxicity assay against human monocytic leukemia (THP-1) cell line. Nano Progress 2021; 3(6): 1–6. doi: 10.36686/Ariviyal.NP.2021.03.06.027.
[29]Singh AP, Biswas A, Shukla A, et al. Targeted therapy in chronic diseases using nanomaterial-based drug delivery vehicles. Signal Transduction and Targeted Therapy 2019; 4(33): 1–21. doi: 10.1038/s41392-019-0068-3.
[30]Mitchell MJ, Billingsley MM, Haley RM, et al. Engineering precision nanoparticles for drug delivery. Nature Reviews Drug Discovery 2021; 20(2): 101–124. doi: 10.1038/s41573-020-0090-8.
[31]Madaan K, Kumar S, Poonia N, et al. Dendrimers in drug delivery and targeting: Drug-dendrimer interactions and toxicity issues. Journal of Pharmacy and Bioallied Sciences 2014; 6(3): 139–150. doi: 10.4103/0975-7406.130965.
[32]Wei P, Cornel EJ, Du J. Ultrasound-responsive polymer-based drug delivery systems. Drug Delivery and Translational Research 2021; 11: 1323–1339. doi: 10.1007/s13346-021-00963-0.
[33]Aibani N, Khan TN, Callan B. Liposome mimicking polymersomes: A comparative study of the merits of polymersomes in terms of formulation and stability. International Journal of Pharmaceutics: X 2020; 2: 100040. doi: 10.1016/j.ijpx.2019.100040.
[34]Anajafi T, Mallik S. Polymersome-based drug-delivery strategies for cancer therapeutics. Therapeutic Delivery 2015; 6(4): 521–534. doi: 10.4155/tde.14.125.
[35]Sharma AK, Prasher P, Aljabali AA, et al. Emerging era of “somes”: Polymersomes as versatile drug delivery carrier for cancer diagnostics and therapy. Drug Delivery and Translational Research 2020; 10(5): 1171–1190. doi: 10.1007/s13346-020-00789-2.
[36]Apolinario AC, Ferraro RB, de Oliveira CA, et al. Quality-by-design approach for biological API encapsulation into polymersomes using “off-the-shelf” materials: A study on L-asparaginase. AAPS PharmSciTech 2019; 20(6): 251. doi: 10.1208/s12249-019-1465-1.
[37]Lee JS, Feijen J. Polymersomes for drug delivery: Design, formation and characterization. Journal of Controlled Release 2012; 161(2): 473–483. doi: 10.1016/j.jconrel.2011.10.005.
[38]Hasannia M, Aliabadi A, Abnous K, et al. Synthesis of block copolymers used in polymersome fabrication: Application in drug delivery. Journal of Controlled Release 2022; 341: 95–117. doi: 10.1016/j.jconrel.2021.11.010.
[39]Balasubramanian V, Herranz-Blanco B, Almeida PV, et al. Multifaceted polymersome platforms: Spanning from self-assembly to drug delivery and protocells. Progress in Polymer Science 2016; 60: 51–85. doi: 10.1016/j.progpolymsci.2016.04.004.
[40]Liu Q, Song L, Chen S, et al. A superparamagnetic polymersome with extremely high T2 relaxivity for MRI and cancer-targeted drug delivery. Biomaterials 2017; 114: 23–33. doi: 10.1016/j.biomaterials.2016.10.027.
[41]Zhu D, Wu S, Hu C, et al. Folate-targeted polymersomes loaded with both paclitaxel and doxorubicin for the combination chemotherapy of hepatocellular carcinoma. Acta Biomaterialia 2017; 58: 399–412. doi: 10.1016/j.actbio.2017.06.017.
[42]Deng Z, Hu J, Liu S. Reactive oxygen, nitrogen, and sulfur species (RONSS)—Responsive polymersomes for triggered drug release. Macromolecular Rapid Communications 2017; 38(11): 1600685. doi: 10.1002/marc.201600685.
[43]Deng Y, Chen H, Tao X, et al. Oxidation-sensitive polymersomes based on amphiphilic diblock copolypeptoids. Biomacromolecules 2019; 20(9): 3435–3444. doi: 10.1021/acs.biomac.9b00713.
[44]Li J, Li Y, Wang Y, et al. Polymer prodrug-based nanoreactors activated by tumor acidity for orchestrated oxidation/chemotherapy. Nano Letters 2017; 17(11): 6983–6990. doi: 10.1021/acs.nanolett.7b03531.
[45]Rawding PA, Bu J, Wang J, et al. Dendrimers for cancer immunotherapy: Avidity-based drug delivery vehicles for effective anti-tumor immune response. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology 2022; 14(2): e1752. doi: 10.1002/wnan.1752.
[46]Kannan RM, Nance E, Kannan S, et al. Emerging concepts in dendrimer-based nanomedicine: From design principles to clinical applications. Journal of Internal Medicine 2014; 276(6): 579–617. doi: 10.1111/joim.12280.
[47]Tripathy S, Das MK. Dendrimers and their applications as novel drug delivery carriers. Journal of Applied Pharmaceutical Science 2013; 3(9): 142–149. doi: 10.7324/JAPS.2013.3924.
[48]Khodabakhshi MJ, Panahi HA, Konoz E, et al. Synthesis of pH and thermo-sensitive dendrimers based on MoS2 and magnetic nanoparticles for cisplatin drug delivery system by the near—Infrared laser. Polymers for Advanced Technologies 2020; 32(4): 1626–1635. doi: 10.1002/pat.5199.
[49]Shi Y, Lammers T, Stor G, et al. Physico-chemical strategies to enhance stability and drug retention of polymeric micelles for tumor-targeted drug delivery. Macromolecular Bioscience 2017; 17(1): 1600160. doi: 10.1002/mabi.201600160.
[50]Movassaghian S, Merkel OM, Torchilin VP. Applications of polymer micelles for imaging and drug delivery. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology 2015; 7(5): 691–707. doi: 10.1002/wnan.1332.
[51]Letchford K, Burt H. A review of the formation and classification of amphiphilic block copolymer nanoparticulate structures: Micelles, nanospheres, nanocapsules and polymersomes. European Journal of Pharmaceutics and Biopharmaceutics 2007; 65(3): 259–269. doi: 10.1016/j.ejpb.2006.11.009.
[52]Liao C, Chen Y, Yao Y, et al. Cross-linked small-molecule micelle-based drug delivery system: Concept, synthesis, and biological evaluation. Chemistry of Materials 2016; 28(21): 7757–7764. doi: 10.1021/acs.chemmater.6b02965.
[53]Guo Y, Gao T, Fang F, et al. A novel polymer micelle as a targeted drug delivery system for 10-hydroxycamptothecin with high drug-loading properties and anti-tumor efficacy. Biophysical Chemistry 2021; 279: 106679. doi: 10.1016/j.bpc.2021.106679.
[54]Pham DT, Chokamonsirikun A, Phattaravorakarn V, et al. Polymeric micelles for pulmonary drug delivery: A comprehensive review. Journal of Materials Science 2021; 56(3): 2016–2036. doi: 10.1007/s10853-020-05361-4.
[55]Ghezzi M, Pescina S, Padula C, et al. Polymeric micelles in drug delivery: An insight of the techniques for their characterization and assessment in biorelevant conditions. Journal of Controlled Release 2021; 332: 312–336. doi: 10.1016/j.jconrel.2021.02.031.
[56]Miao Y, Niu X, Wu A, et al. Metallic oxide-induced self-assembly of block copolymers to form polymeric hybrid micelles with tunable stability for tumor microenvironment-responsive drug delivery. ACS Applied Materials & Interfaces 2021; 13(28): 32753–32762. doi: 10.1021/acsami.1c07168.
[57]García MC. Nano-and microparticles as drug carriers. Engineering drug delivery systems. Cambridgeshire: Woodhead Publishing; 2020. p. 71–110. doi: 10.1016/B978-0-08-102548-2.00004-4.
[58]Pada AK, Desai D, Sun K, et al. Comparison of polydopamine-coated mesoporous silica nanorods and spheres for the delivery of hydrophilic and hydrophobic anticancer drugs. International Journal of Molecular Sciences 2019; 20(14): 3408. doi: 10.3390/ijms20143408.
[59]Lotfalian S, Nematollahzadeh A, Ghasemi S. Hierarchically structured protein-based hollow-nanospheres for drug delivery. Reactive and Functional Polymers 2021; 160: 104821. doi: 10.1016/j.reactfunctpolym.2021.104821.
[60]Geyik G, Işıklan N. Design and fabrication of hybrid triple-responsive κ-carrageenan-based nanospheres for controlled drug delivery. International Journal of Biological Macromolecules 2021; 192: 701–715. doi: 10.1016/j.ijbiomac.2021.10.007.
[61]Das MP, Pandey G, Neppolian B, et al. Design of poly-l-glutamic acid embedded mesoporous bioactive glass nanospheres for pH-stimulated chemotherapeutic drug delivery and antibacterial susceptibility. Colloids and Surfaces B: Biointerfaces 2021; 202: 111700. doi: 10.1016/j.colsurfb.2021.111700.
[62]Uson L, Yus C, Mendoza G, et al. Nanoengineering palladium plasmonic nanosheets inside polymer nanospheres for photothermal therapy and targeted drug delivery. Advanced Functional Materials 2022; 32(9): 2106932. doi: 10.1002/adfm.202106932.
[63]Wang M, Yang D, Xu Q, et al. Highly efficient evaporation method to prepare pH-responsive lignin-hollow-nanosphere with controllable size and its application in oral drug delivery. Industrial Crops and Products 2021; 162: 113230. doi: 10.1016/j.indcrop.2020.113230.
[64]Boltnarova B, Kubackova J, Skoda J, et al. PLGA based nanospheres as a potent macrophage-specific drug delivery system. Nanomaterials 2021; 11(3): 749. doi: 10.3390/nano11030749.
[65]Liu J, Cui Y, Kuang Y, et al. Hierarchically porous calcium–silicon nanosphere-enabled co-delivery of microRNA-210 and simvastatin for bone regeneration. Journal of Materials Chemistry B 2021; 9(16): 3573–3583. doi: 10.1039/D1TB00063B.
[66]Zhang K, Zhang Y, Li Y, et al. The thermal/pH-sensitive drug delivery system encapsulated by PAA based on hollow hybrid nanospheres with two silicon source. Journal of Biomaterials Science, Polymer Edition 2021; 32(6): 695–713. doi: 10.1080/09205063.2020.1861734.
[67]Li L, Yu C, Yu C, et al. Nanocellulose as template to prepare rough-hydroxy rich hollow silicon mesoporous nanospheres (R-nCHMSNs) for drug delivery. International Journal of Biological Macromolecules 2021; 180: 432–438. doi: 10.1016/j.ijbiomac.2021.03.031.
[68]De Gaetano F, Marino A, Marchetta A, et al. Development of chitosan/cyclodextrin nanospheres for levofloxacin ocular delivery. Pharmaceutics 2021; 13(8): 1293. doi: 10.3390/pharmaceutics13081293.
[69]Elkayal R, Motawea A, Reicha FM, et al. Novel electro self-assembled DNA nanospheres as a drug delivery system for atenolol. Nanotechnology 2021; 32(25): 255602. doi: 10.1088/1361-6528/abd727.
[70]Neamtu I, Rusu AG, Diaconu A, et al. Basic concepts and recent advances in nanogels as carriers for medical applications. Drug Delivery 2017; 24(1): 539–557. doi: 10.1080/10717544.2016.1276232.
[71]Soni KS, Desale SS, Bronich TK. Nanogels: An overview of properties, biomedical applications and obstacles to clinical translation. Journal of Controlled Release 2016; 240: 109–126. doi: 10.1016/j.jconrel.2015.11.009.
[72]Li Z, Huang J, Wu J. PH-sensitive nanogels for drug delivery in cancer therapy. Biomaterials Science 2021; 9(3): 574–589. doi: 10.1039/d0bm01729a.
[73]Limiti E, Mozetic P, Giannitelli SM, et al. Hyaluronic acid–polyethyleneimine nanogels for controlled drug delivery in cancer treatment. ACS Applied Nano Materials 2022; 5(4): 5544–5557. doi: 10.1021/acsanm.2c00524.
[74]Pooresmaeil M, Namazi H, Salehi R. Dual anticancer drug delivery of D-galactose-functionalized stimuli-responsive nanogels for targeted therapy of the liver hepatocellular carcinoma. European Polymer Journal 2022; 167: 111061. doi: 10.1016/j.eurpolymj.2022.111061.
[75]Alyassin Y, Sayed EG, Mehta P, et al. Application of mesoporous silica nanoparticles as drug delivery carriers for chemotherapeutic agents. Drug Discovery Today 2020; 25(8): 1513–1520. doi: 10.1016/j.drudis.2020.06.006.
[76]Zhang B, Chen X, Fan X, et al. Lipid/PAA-coated mesoporous silica nanoparticles for dual-pH-responsive codelivery of arsenic trioxide/paclitaxel against breast cancer cells. Acta Pharmacologica Sinica 2021; 42(5): 832–842. doi: 10.1038/s41401-021-00648-x.
[77]Wang Y, Zhao Q, Han N, et al. Mesoporous silica nanoparticles in drug delivery and biomedical applications. Nanomedicine: Nanotechnology, Biology and Medicine 2015; 11(2): 313–327. doi: 10.1016/j.nano.2014.09.014.
[78]Argyo C, Weiss V, Bräuchle C, et al. Multifunctional mesoporous silica nanoparticles as a universal platform for drug delivery. Chemistry of Materials 2013; 26(1): 435–451. doi: 10.1021/cm402592t.
[79]Bharti C, Nagaich U, Pal AK, et al. Mesoporous silica nanoparticles in target drug delivery system: A review. International Journal of Pharmaceutical Investigation 2015; 5(3): 124–133. doi: 10.4103/2230-973X.160844.
[80]Vallet-Regí M, Colilla M, Izquierdo-Barba I, et al. Mesoporous silica nanoparticles for drug delivery: Current insights. Molecules 2017; 23(1): 47. doi: 10.3390/molecules23010047.
[81]Bagheri E, Alibolandi M, Abnous K, et al. Targeted delivery and controlled release of doxorubicin to cancer cells by smart ATP-responsive Y-shaped DNA structure-capped mesoporous silica nanoparticles. Journal of Materials Chemistry B 2021; 9: 1351–1363. doi: 10.1039/D0TB01960G.
[82]Harun SN, Ahmad H, Lim HN, et al. Synthesis and optimization of mesoporous silica nanoparticles for ruthenium polypyridyl drug delivery. Pharmaceutics 2021; 13(2): 150. doi: 10.3390/pharmaceutics13020150.
[83]Murugan B, Krishnan UM. Differently sized drug-loaded mesoporous silica nanoparticles elicit differential gene expression in MCF-7 cancer cells. Nanomedicine 2021; 16(12): 1017–1034. doi: 10.2217/nnm-2020-0375.
[84]Prabha S, Durgalakshmi D, Rajendran S, et al. Plant-derived silica nanoparticles and composites for biosensors, bioimaging, drug delivery and supercapacitors: A review. Environmental Chemistry Letters 2021; 19(2): 1667–1691. doi: 10.1007/s10311-020-01123-5.
[85]Nemati A. Quantum dots in therapeutic, diagnostic and drug delivery applications “a brief review”. Iranian Journal of Materials Science and Engineering 2020; 17(2): 80–91. doi: 10.22068/ijmse.17.2.1.
[86]Ghahramani Y, Javanmardi N. Graphene oxide quantum dots and their applications via stem cells: A mini-review. Advances in Applied NanoBio-Technologies 2021; 2(3): 54–56. doi: 10.47277/AANBT/2(3)56.
[87]Biswas MC, Islam MT, Nandy PK, Hossain MM. Graphene quantum dots (GQDs) for bioimaging and drug delivery applications: A review. ACS Materials Letters 2021; 3: 889–911. doi: 10.1021/acsmaterialslett.0c00550.
[88]Zhao C, Song X, Liu Y, et al. Synthesis of graphene quantum dots and their applications in drug delivery. Journal of Nanobiotechnology 2020; 18(1): 142. doi: 10.1186/s12951-020-00698-z.
[89]Badıllı U, Mollarasouli F, Bakirhan NK, et al. Role of quantum dots in pharmaceutical and biomedical analysis, and its application in drug delivery. TrAC Trends in Analytical Chemistry 2020; 131: 116013. doi: 10.1016/j.trac.2020.116013.
[90]Probst CE, Zrazhevskiy P, Bagalkot V, et al. Quantum dots as a platform for nanoparticle drug delivery vehicle design. Advanced Drug Delivery Reviews 2013; 65(5): 703–718. doi: 10.1016/j.addr.2012.09.036.
[91]Henna TK, Pramod K. Graphene quantum dots redefine nanobiomedicine. Materials Science and Engineering 2020; 110: 110651. doi: 10.1016/j.msec.2020.110651.
[92]Li Z, Fan J, Tong C, et al. A smart drug-delivery nanosystem based on carboxylated graphene quantum dots for tumor-targeted chemotherapy. Nanomedicine 2019; 14(15): 2011–2025. doi: 10.2217/nnm-2018-0378.
[93]Ghanbari N, Salehi Z, Khodadadi AA, et al. Tryptophan-functionalized graphene quantum dots with enhanced curcumin loading capacity and pH-sensitive release. Journal of Drug Delivery Science and Technology 2021; 61: 102137. doi: 10.1016/j.jddst.2020.102137.
[94]Wang X, Sun X, Lao J, et al. Multifunctional graphene quantum dots for simultaneous targeted cellular imaging and drug delivery. Colloids and Surfaces B: Biointerfaces 2014; 122: 638–644. doi: 10.1016/j.colsurfb.2014.07.043.
[95]Yu C, Long Z, Qiu Q, et al. Graphene quantum dots—Based targeted nanoprobes detecting drug delivery, imaging and enhanced chemotherapy of nasopharyngeal carcinoma. Bioengineering and Translational Medicine 2021; 7(2): e10270. doi: 10.1002/btm2.10270.
[96]Tade RS, More MP, Nangare SN, et al. Graphene quantum dots (GQDs) nanoarchitectonics for theranostic application in lung cancer. Journal of Drug Targeting 2022; 30(3): 269–286. doi: 10.1080/1061186X.2021.1987442.
[97]Liu Y, Huang H, Cao W, et al. Advances in carbon dots: From the perspective of traditional quantum dots. Materials Chemistry Frontiers 2020; 4(6): 1586–1613. doi: 10.1039/D0QM00090F.
[98]Khan ZG, Patil PO. A comprehensive review on carbon dots and graphene quantum dots based fluorescent sensor for biothiols. Microchemical Journal 2020; 157: 105011. doi: 10.1016/j.microc.2020.105011.
[99]Das P, Ganguly S, Agarwal T, et al. Heteroatom doped blue luminescent carbon dots as a nano-probe for targeted cell labeling and anticancer drug delivery vehicle. Materials Chemistry and Physics 2019; 237: 121860. doi: 10.1016/j.matchemphys.2019.121860.
[100]Hettiarachchi SD, Graham RM, Mintz KJ, et al. Triple conjugated carbon dots as a nano-drug delivery model for glioblastoma brain tumors. Nanoscale 2019; 11(13): 6192–6205. doi: 10.1039/c8nr08970a.
[101]Ganguly S, Das P, Itzhaki E, et al. Microwave-synthesized polysaccharide-derived carbon dots as therapeutic cargoes and toughening agents for elastomeric gels. ACS Applied Materials & Interfaces 2020; 12(46): 51940–51951. doi: 10.1021/acsami.0c14527.
[102]Huang H, Dong C, Feng W, et al. Biomedical engineering of two-dimensional MXenes. Advanced Drug Delivery Reviews 2022; 184: 114178. doi: 10.1016/j.addr.2022.114178.
[103]Tareen AK, Khan K, Iqbal M, et al. Recent advances in MXenes: New horizons in biomedical technologies. Materials Today Chemistry 2022; 26: 101205. doi: 10.1016/j.mtchem.2022.101205.
[104]Sivasankarapillai VS, Somakumar AK, Joseph J, et al. Cancer theranostic applications of MXene nanomaterials: Recent updates. Nano-Structures & Nano-Objects 2020; 22: 100457. doi: 10.1016/j.nanoso.2020.100457.
[105]Iravani S, Varma RS. Smart MXene quantum dot-based nanosystems for biomedical applications. Nanomaterials 2022; 12(7): 1200. doi: 10.3390/nano12071200.
[106]Iravani S, Varma RS. MXenes in photomedicine: Advances and prospects. Chemical Communications 2022; 58(53): 7336–7350. doi: 10.1039/d2cc01694j.
[107]Iravani S. MXenes and MXene-based (nano) structures: A perspective on greener synthesis and biomedical prospects. Ceramics International 2022; 48(17): 24144–24156. doi: 10.1016/j.ceramint.2022.05.137.
[108]Turrina C, Berensmeier S, Schwaminger SP. Bare iron oxide nanoparticles as drug delivery carrier for the short cationic peptide lasioglossin. Pharmaceuticals 2021; 14(5): 405. doi: 10.3390/ph14050405.
[109]Chertok B, Moffat BA, David AE, et al. Iron oxide nanoparticles as a drug delivery vehicle for MRI monitored magnetic targeting of brain tumors. Biomaterials 2008; 29(4): 487–496. doi: 10.1016/j.biomaterials.2007.08.050.
[110]Cotta KB, Mehra S, Bandyopadhyaya R. PH-driven enhancement of anti-tubercular drug loading on iron oxide nanoparticles for drug delivery in macrophages. Beilstein Journal of Nanotechnology 2021; 12(1): 1127–1139. doi: 10.3762/bjnano.12.84.
[111]Yuan A, Ruan L, Ji R, et al. Tumor exosome-mimicking iron oxide nanoparticles for near infrared-responsive drug delivery. ACS Applied Nano Materials 2021; 5(1): 996–1002. doi: 10.1021/acsanm.1c03643.
[112]Nedyalkova M, Todorov B, Barazorda-Ccahuanac HL, et al. Iron oxide nanoparticles in anticancer drug delivery and imaging diagnostics. 1st ed. In: Caizer C, Rai M (editors). Magnetic nanoparticles in human health and medicine: Current medical applications and alternative therapy of cancer. New Jersey: Wiley-Blackwell; 2021. p. 151–163.
[113]Barkhordari S, Alizadeh A, Yadollahi, et al. One-pot synthesis of magnetic chitosan/iron oxide bio-nanocomposite hydrogel beads as drug delivery systems. Soft Materials 2020; 19(4): 373–381. doi: 10.1080/1539445X.2020.1829642.
[114]Rezaei A, Morsali A, Bozorgmehr MR, Nasrabadi M. Quantum chemical analysis of 5-aminolevulinic acid anticancer drug delivery systems: Carbon nanotube, –COOH functionalized carbon nanotube and iron oxide nanoparticle. Journal of Molecular Liquids 2021; 340: 117182. doi: 10.1016/j.molliq.2021.117182.
[115]Gutiérrez-Romero L, Rivas-García L, Sánchez-González C, et al. Cellular toxicity mechanisms and the role of autophagy in Pt (IV) prodrug-loaded ultrasmall iron oxide nanoparticles used for enhanced drug delivery. Pharmaceutics 2021; 13(10): 1730. doi: 10.3390/pharmaceutics13101730.
[116]Turiel-Fernández D, Gutiérrez-Romero L, Corte-Rodriguez M, et al. Ultrasmall iron oxide nanoparticles cisplatin (IV) prodrug nanoconjugate: ICP-MS based strategies to evaluate the formation and drug delivery capabilities in single cells. Analytica Chimica Acta 2021; 1159: 338356. doi: 10.1016/j.aca.2021.338356.
[117]Nejati K, Dadashpou M, Gharibi T, et al. Biomedical applications of functionalized gold nanoparticles: A review. Journal of Cluster Science 2021; 33(1): 1–16. doi: 10.1007/s10876-020-01955-9.
[118]Yafout M, Ousaid A, Khayati Y, et al. Gold nanoparticles as a drug delivery system for standard chemotherapeutics: A new lead for targeted pharmacological cancer treatments. Scientific African 2021; 11: e00685. doi: 10.1016/j.sciaf.2020.e00685.
[119]Lacroce E, Saccomandi P, Rossi F. Can gold nanoparticles improve delivery performance of polymeric drug-delivery systems? Therapeutic Delivery 2021; 12(7): 489–492. doi: 10.4155/tde-2021-0037.
[120]Horo H, Bhattacharyya S, Mandal B, et al. Synthesis of functionalized silk-coated chitosan-gold nanoparticles and microparticles for target-directed delivery of antitumor agents. Carbohydrate Polymers 2021; 258: 117659. doi: 10.1016/j.carbpol.2021.117659.
[121]Huang Y, Yu F, Park Y S, et al. Co-administration of protein drugs with gold nanoparticles to enable percutaneous delivery. Biomaterials 2010; 31(34): 9086–9091. doi: 10.1016/j.biomaterials.2010.08.046.
[122]Sulaiman GM, Waheeb HM, Jabir MS, et al. Hesperidin loaded on gold nanoparticles as a drug delivery system for a successful biocompatible, anti-cancer, anti-inflammatory and phagocytosis inducer model. Scientific Reports 2020; 10(1): 9362. doi: 10.1038/s41598-020-66419-6.
[123]Essawy MM, El-Sheikh SM, Raslan HS, et al. Function of gold nanoparticles in oral cancer beyond drug delivery: Implications in cell apoptosis. Oral Diseases 2021; 27(2): 251–265. doi: 10.1111/odi.13551.
[124]Dreaden EC, Austin LA, Mackey MA, El-Sayed MA. Size matters: Gold nanoparticles in targeted cancer drug delivery. Therapeutic Delivery 2012; 3: 457–478. doi: 10.4155%2Ftde.12.21.
[125]Khodashenas B, Ardjmand M, Rad AS, et al. Gelatin-coated gold nanoparticles as an effective pH-sensitive methotrexate drug delivery system for breast cancer treatment. Materials Today Chemistry 2021; 20: 100474. doi: 10.1016/j.mtchem.2021.100474.
[126]Hassanen EI, Korany RM, Bakeer AM. Cisplatin-conjugated gold nanoparticles-based drug delivery system for targeting hepatic tumors. Journal of Biochemical and Molecular Toxicology 2021; 35(5): e22722. doi: 10.1002/jbt.22722.
[127]Jha B, Prasad K, Jha AK. Cytotoxicity of biogenic gold nanoparticles against lung cancer cell line (A549): An application oriented perspective. Preprints.org 2018. doi: 10.20944/preprints201812.0308.v1.
[128]Fonseca-Santos B, Gremião MPD, Chorilli M. Nanotechnology-based drug delivery systems for the treatment of Alzheimer’s disease. International Journal of Nanomedicine 2015; 10: 4981–5003. doi: 10.2147/IJN.S87148.
[129]Moulahoum H, Ghorbanizamani F, Zihnioglu F, et al. Surface biomodification of liposomes and polymersomes for efficient targeted drug delivery. Bioconjugate Chemistry 2021; 32(8): 1491–1502. doi: 10.1021/acs.bioconjchem.1c00285.
[130]Osorno LL, Brandley AN, Maldonado DE, et al. Review of contemporary self-assembled systems for the controlled delivery of therapeutics in medicine. Nanomaterials 2021; 11(2): 278. doi: 10.3390/nano11020278.
[131]Hare JI, Lammers T, Ashford MB, et al. Challenges and strategies in anti-cancer nanomedicine development: An industry perspective. Advanced Drug Delivery Reviews 2017; 108: 25–38. doi: 10.1016/j.addr.2016.04.025.
[132]Markman M. Pegylated liposomal doxorubicin in the treatment of cancers of the breast and ovary. Expert Opinion on Pharmacotherapy 2006; 7(11): 1469–1474. doi: 10.1517/14656566.7.11.1469.
[133]Sarfraz M, Afzal A, Yang T, et al. Development of dual drug loaded nanosized liposomal formulation by a reengineered ethanolic injection method and its pre-clinical pharmacokinetic studies. Pharmaceutics 2018; 10(3): 151. doi: 10.3390/pharmaceutics10030151.
[134]Edis Z, Wang J, Waqas MK, et al. Nanocarriers-mediated drug delivery systems for anticancer agents: An overview and perspectives. International Journal of Nanomedicine 2021; 16: 1313–1330. doi: 10.2147/IJN.S289443.
[135]Li H, Di J, Peng B, et al. Surface ligand valency and immunoliposome binding: When more is not always better. Pharmaceutical Research 2021; 38(9): 1593–1600. doi: 10.1007/s11095-021-03092-y.
[136]Feng B, Tomizawa K, Michiue H, et al. Development of a bifunctional immunoliposome system for combined drug delivery and imaging in vivo. Biomaterials 2010; 31(14): 4139–4145. doi: 10.1016/j.biomaterials.2010.01.086.
[137]Loureiro JA, Gomes B, Fricker G, et al. Dual ligand immunoliposomes for drug delivery to the brain. Colloids and Surfaces B: Biointerfaces 2015; 134: 213–219. doi: 10.1016/j.colsurfb.2015.06.067.
[138]Tuffin G, Waelti E, Huwyler J, et al. Immunoliposome targeting to mesangial cells: A promising strategy for specific drug delivery to the kidney. Journal of the American Society of Nephrology 2005; 16(11): 3295–3305. doi: 10.1681/ASN.2005050485.
[139]Hamamichi S, Fukuhara T, Umeda IO, et al. Novel method for screening functional antibody with comprehensive analysis of its immunoliposome. Scientific Reports 2021; 11(1): 4625. doi: 10.1038/s41598-021-84043-w.
[140]Yu B, Mao Y, Yuan Y, et al. Targeted drug delivery and cross-linking induced apoptosis with anti-CD37 based dual-ligand immunoliposomes in B chronic lymphocytic leukemia cells. Biomaterials 2013; 34(26): 6185–6193. doi: 10.1016/j.biomaterials.2013.04.063.
[141]Nowroozi F, Almasi A, Javidi J, et al. Effect of surfactant type, cholesterol content and various downsizing methods on the particle size of niosomes. Iranian Journal of Pharmaceutical Research 2018; 17: 1–11.
[142]Yasamineh S, Yasamineh P, Kalajahi HG, et al. A state-of-the-art review on the recent advances of niosomes as a targeted drug delivery system. International Journal of Pharmaceutics 2022; 624: 121878. doi: 10.1016/j.ijpharm.2022.121878.
[143]Sharma R, Dua JS, Parsad DN. An overview on niosomes: Novel pharmaceutical drug delivery system. Journal of Drug Delivery and Therapeutics 2022; 12(2–S): 171–177. doi: 10.22270/jddt.v12i2-S.5264.
[144]Witika BA, Bassey KE, Demana PH, et al. Current advances in specialised niosomal drug delivery: Manufacture, characterization and drug delivery applications. International Journal of Molecular Sciences 2022; 23(17): 9668. doi: 10.3390/ijms23179668.
[145]Aparajay P, Dev A. Functionalized niosomes as a smart delivery device in cancer and fungal infection. European Journal of Pharmaceutical Sciences 2022; 168: 106052. doi: 10.1016/j.ejps.2021.106052.
[146]Rad ME, Egil AC, Ince GO, et al. Optimization of curcumin loaded niosomes for drug delivery applications. Colloids and Surfaces A: Physicochemical and Engineering Aspects 2022; 654: 129921. doi: 10.1016/j.colsurfa.2022.129921.
[147]Naseroleslami M, Niri NM, Akbarzade I, et al. Simvastatin-loaded nano-niosomes confer cardioprotection against myocardial ischemia/reperfusion injury. Drug Delivery and Translational Research 2022; 12(6): 1423–1432. doi: 10.1007/s13346-021-01019-z.
[148]Leung AK, Tam YYC, Chen S, et al. Microfluidic mixing: A general method for encapsulating macromolecules in lipid nanoparticle systems. The Journal of Physical Chemistry B 2015; 119(28): 8698–8706. doi: 10.1021/acs.jpcb.5b02891.
[149]Fenton OS, Olafson KN, Pillai PS, et al. Advances in biomaterials for drug delivery. Advanced Materials 2018; 30(29): 1705328. doi: 10.1002/adma.201705328.
[150]Vhora I, Lalani R, Bhatt P, et al. Lipid-nucleic acid nanoparticles of novel ionizable lipids for systemic BMP-9 gene delivery to bone-marrow mesenchymal stem cells for osteoinduction. International Journal of Pharmaceutics 2019; 563: 324–336. doi: 10.1016/j.ijpharm.2019.04.006.
[151]Patel S, Ryals RC, Weller KK, et al. Lipid nanoparticles for delivery of messenger RNA to the back of the eye. Journal of Controlled Release 2019; 303: 91–100. doi: 10.1016/j.jconrel.2019.04.015.
[152]Fan Y, Marioli M, Zhang K. Analytical characterization of liposomes and other lipid nanoparticles for drug delivery. Journal of Pharmaceutical and Biomedical Analysis 2021; 192: 113642. doi: 10.1016/j.jpba.2020.113642.
[153]Basha SK, Dhandayuthabani R, Muzammil MS, et al. Solid lipid nanoparticles for oral drug delivery. Materials Today: Proceedings 2021; 36: 313–324. doi: 10.1016/j.matpr.2020.04.109.
[154]Satapathy MK, Yen TL, Jan JS, et al. Solid lipid nanoparticles (SLNs): An advanced drug delivery system targeting brain through BBB. Pharmaceutics 2021; 13(8): 1183. doi: 10.3390/pharmaceutics13081183.
[155]Rampaka R, Ommi K, Chella N. Role of solid lipid nanoparticles as drug delivery vehicles on the pharmacokinetic variability of Erlotinib HCl. Journal of Drug Delivery Science and Technology 2021; 66: 102886. doi: 10.1016/j.jddst.2021.102886.
[156]Wiemann S, Keck CM. Are lipid nanoparticles really superior? A holistic proof of concept study. Drug Delivery and Translational Research 2022; 12(6): 1433–1444. doi: 10.1007/s13346-021-01021-5.
[157]Mahmoudian M, Dizaj SM, Salatin S, et al. Oral delivery of solid lipid nanoparticles: Underlining the physicochemical characteristics and physiological condition affecting the lipolysis rate. Expert Opinion on Drug Delivery 2021; 18(11): 1707–1722. doi: 10.1080/17425247.2021.1982891.
[158]Wilson RJ, Li Y, Yang G, et al. Nanoemulsions for drug delivery. Particuology 2022; 64: 85–97. doi: 10.1016/j.partic.2021.05.009.
[159]Hort MA, Alves BDS, Ramires Junior OV, et al. In vivo toxicity evaluation of nanoemulsions for drug delivery. Drug and Chemical Toxicology 2021; 44(6): 585–594. doi: 10.1080/01480545.2019.1659806.
[160]Choradiya BR, Patil SB. A comprehensive review on nanoemulsion as an ophthalmic drug delivery system. Journal of Molecular Liquids 2021; 339: 116751. doi: 10.1016/j.molliq.2021.116751.
[161]Tayeb HH, Sainsbury F. Nanoemulsions in drug delivery: Formulation to medical application. Nanomedicine 2018; 13(19): 2507–2525. doi: 10.2217/nnm-2018-0088.
[162]Sarheed O, Dibi M, Ramesh KV, et al. Fabrication of alginate-based O/W nanoemulsions for transdermal drug delivery of lidocaine: Influence of the oil phase and surfactant. Molecules 2021; 26(9): 2556. doi: 10.3390/molecules26092556.
[163]Cunha S, Forbes B, Lobo JMS, et al. Improving drug delivery for Alzheimer’s disease through nose-to-brain delivery using nanoemulsions, nanostructured lipid carriers (NLC) and in situ hydrogels. International Journal of Nanomedicine 2021; 16: 4373–4390. doi: 10.2147/IJN.S305851.
[164]D’Arrigo JS. Biobased nanoemulsion methodology aimed at nanotargeted drug delivery for dementia. Nano Progress 2021: 3(6): 11–18. doi: 10.36686/Ariviyal.NP.2021.03.06.029.
[165]Tedesco AC, Silva EP, Jayme CC, et al. Cholesterol-rich nanoemulsion (LDE) as a novel drug delivery system to diagnose, delineate, and treat human glioblastoma. Materials Science and Engineering: C 2021; 123: 111984. doi: 10.1016/j.msec.2021.111984.
[166]Hu Q, Lu Y, Luo Y. Recent advances in dextran-based drug delivery systems: From fabrication strategies to applications. Carbohydrate Polymers 2021; 264: 117999. doi: 10.1016/j.carbpol.2021.117999.
[167]Kleinubing SA, Outuki PM, Hoscheid J, et al. Hyaluronic acid incorporation into nanoemulsions containing Pterodon pubescens Benth. Fruit oil for topical drug delivery. Biocatalysis and Agricultural Biotechnology 2021; 32: 101939. doi: 10.1016/j.bcab.2021.101939.
[168]Schütz CA, Juillerat-Jeanneret L, Mueller H, et al. Therapeutic nanoparticles in clinics and under clinical evaluation. Nanomedicine 2013; 8(3): 449–467. doi: 10.2217/nnm.13.8.
[169]Jain K, Kumar Mehra N, Jain NK. Nanotechnology in drug delivery: Safety and toxicity issues. Current Pharmaceutical Design 2015; 21(29): 4252–4261. doi: 10.2174/1381612821666150901103208.
[170]Yuan Y, Ding J, Xu J, et al. TiO2 nanoparticles co-doped with silver and nitrogen for antibacterial application. Journal of Nanoscience and Nanotechnology 2010; 10(8): 4868–4874. doi: 10.1166/jnn.2010.2225.
[171]Kozma G, Shimizu T, Ishida T, et al. Anti-PEG antibodies: Properties, formation and role in adverse immune reactions to PEGylated nano-biopharmaceuticals. Advanced Drug Delivery Reviews 2020; 154–155: 163–175. doi: 10.1016/j.addr.2020.07.024.
[172]Pease DF, Peterson BA, Gilles S, et al. Development of cutaneous squamous cell carcinoma after prolonged exposure to pegylated liposomal doxorubicin and hand-foot syndrome: A newly recognized toxicity. Cancer Chemotherapy and Pharmacology 2019; 84(1): 217–221. doi: 10.1007/s00280-019-03849-8.
[173]Najahi-Missaoui W, Arnold RD, Cummings BS. Safe nanoparticles: Are we there yet? International Journal of Molecular Sciences 2020; 22(1): 385. doi: 10.3390/ijms22010385.
[174]Herrmann IK, Wood MJA, Fuhrmann G. Extracellular vesicles as a next-generation drug delivery platform. Nature Nanotechnology 2021; 16(7): 748–759. doi: 10.1038/s41565-021-00931-2.
Copyright (c) 2024 Manisha Mishra, Kamal Prasad, S. Ramakrishna, Anal Kant Jha

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Authors contributing to this journal agree to publish their articles under the Creative Commons Attribution 4.0 International License, allowing third parties to share their work (copy, distribute, transmit) and to adapt it for any purpose, even commercially, under the condition that the authors are given credit. With this license, authors hold the copyright.